X-ray, thanks for the X-ray!
More than half the length of the tooth is hidden under soft and hard tissues.
Wilhelm Conrad Roentgen
Unable to “see through” doctors could only guess at the causes of diseases, until in 1895 the discovery of the German scientist Wilhelm Conrad Roentgen changed the approach to diagnosing injuries and diseases. You can read about the history of the discovery of X-rays on Wikipedia.
The rays discovered by Roentgen, which he called X-ray (“unknown” rays), had the ability to penetrate various objects: paper, wood, layers of metal and the human body.
X-rays passing through objects of different densities
Objects with a dense structure (for example, human bones) transmitted rays worse than less dense objects (for example, soft tissue). This feature formed the basis for diagnosing the causes of various diseases that are invisible during visual examination.
Just a year after the discovery of X-rays, devices based on them were used to diagnose bone fractures. In 1901, Wilhelm Conrad Roentgen received the Nobel Prize in Physics for his discovery of “unknown” rays.
X-ray examination
RADIOSCOPE (transmission) is a method of X-ray examination in which, using X-rays, a positive image of the object under study is obtained on a fluorescent screen. One of the main methods of x-ray diagnostics. During fluoroscopy, dense areas of the object (bones, foreign bodies) appear dark, less dense areas (soft tissue) appear lighter.
The main advantage of fluoroscopy is the fact that it can be examined in real time. This allows you to evaluate not only the structure of the organ, but also its displacement, contractility or distensibility, passage of the contrast agent, and filling. The method also allows you to quickly assess the localization of some changes, due to the rotation of the object of study during transillumination. Fluoroscopy allows you to monitor the implementation of some instrumental procedures - placement of catheters, angioplasty, fistulography.
The main differences of digital fluoroscopy are the use of modern X-ray detectors and the ability to digitally process an X-ray image while simultaneously displaying it on a monitor screen or in an image recording device. With the advent of digital technologies, 3 main disadvantages inherent in traditional fluoroscopy have disappeared:
- Relatively high radiation dose compared to radiography - modern low-dose devices have left this disadvantage in the past. The use of pulsed scanning modes further reduces the dose load by up to 90%.
- Low spatial resolution - on modern digital devices, the resolution in the copy mode is only slightly inferior to the resolution in the radiographic mode. In this case, the ability to observe the functional state of individual organs (heart, lungs, stomach, intestines) “in dynamics” is of decisive importance.
- The impossibility of documenting research - digital image processing technologies make it possible to save research materials, both frame-by-frame and in the form of a video sequence. The resulting images can be placed on a regular CD or in network storage.
Fluoroscopy is performed mainly for X-ray diagnosis of diseases of internal organs located in the abdominal and thoracic cavities, according to the plan that the radiologist draws up before the start of the study. Sometimes, the so-called survey fluoroscopy is used to recognize traumatic bone injuries, to clarify the area to be radiographed.
In contrast to the organs of the chest, which are a favorable object for x-ray examination, the abdominal cavity with its contents and the organs of the retroperitoneal space, due to x-ray anatomical features, are not differentiated with conventional fluoroscopy. If the shadow of the heart is clearly visible against the background of transparent pulmonary fields, and the elements of the bony skeleton clearly appear against the background of soft tissues, then to identify the liver, biliary tract, spleen, gastrointestinal tract, urinary tract against the background of the surrounding soft tissues and organs, they usually resort to contrasting research methods.
Contrast fluoroscopic examination
Artificial contrast extremely expands the possibilities of fluoroscopic examination of organs and systems where tissue densities are approximately the same (for example, the abdominal cavity, the organs of which transmit X-ray radiation to approximately the same extent and are therefore low-contrast). This is achieved by introducing into the lumen of the stomach or intestines an aqueous suspension of barium sulfate, which does not dissolve in digestive juices, is not absorbed by either the stomach or intestines and is excreted naturally in a completely unchanged form. The main advantage of a barium suspension is that, passing through the esophagus, stomach and intestines, it coats their internal walls and gives on a screen or film a complete picture of the nature of the elevations, depressions and other features of their mucous membrane. The study of the internal relief of the esophagus, stomach and intestines helps to recognize a number of diseases of these organs. With tighter filling, the shape, size, position and function of the organ under study can be determined.
, double contrast is often used . To do this, additional air is introduced into the organ being examined. In this case, a small amount of high-density barium covers the surface of the mucous membrane, and the introduction of gas inflates the organ, increasing the contrast. In some cases, to study the walls of the stomach between two air environments, oxygen is injected into the abdominal cavity.
The main contraindication to X-ray contrast studies is the suspicion of perforation, since free barium is a strong irritant to the mediastinum and peritoneum; water-soluble contrast agent is less irritating and can be used if perforation is suspected.
More information about contrast agents can be found in the special section Radiocontrast agents
To examine the colon, irrigoscopy , which consists of injecting an aqueous suspension of barium sulfate into it using an enema after preliminary cleansing of the intestine.
During fluoroscopy of the esophagus, stomach and duodenum, the patient is given a radiopaque mixture to drink before the examination. In this case, special mixtures based on barium sulfate with flavoring additives are used.
The fluoroscopy techniques of the esophagus, stomach, and intestines have been worked out in great detail. They are safe and easy for the patient. The diagnostic value of scopic examinations is extremely high. For millions of patients, doctors annually conduct fluoroscopic examinations of organs, both to establish a diagnosis of the disease and to monitor the results of treatment.
Registration and preparation for complex studies (stomach x-ray, urography, irrigoscopy, etc.) must be discussed with the x-ray laboratory assistant.
Equipment for X-ray diagnostics
For a long time, the results of the passage of X-rays through objects of various densities were recorded on photographic film.

Today, most X-ray diagnostic devices use digital sensors instead of photographic film, so the image can be immediately seen on a computer screen, and, if necessary, saved to a file or printed on a printer.
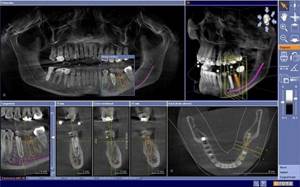
To make a diagnosis, plan treatment, monitor treatment progress, and check treatment results, dentists can use three types of x-ray equipment:
- radiovisiographs (image of 1-3 teeth)
- orthopontamographs (panoramic images of the jaws)
- computed tomography scans (three-dimensional images of the jaws)
Orthopantomograph – an opportunity to see the “big picture”

An orthopantomogram is a panoramic photograph of the upper and lower jaw. This type of x-ray examination is needed to see the general condition of the dental system, so a consultation with a dentist often begins with this image.

The panoramic image clearly shows “live” and pulpless teeth, foci of chronic infection, the level of bone tissue, periodontal pockets and much more.

change of teeth in a panoramic photograph
Radiation methods used in dentistry
Information is presented on the basic and special methods of radiation examination used in the diagnosis of diseases of the maxillofacial region. The diagnostic capabilities of the methods are reviewed and indications for their use are determined. The capabilities of modern methods - computed tomography, ultrasound - are also covered.

X-ray research methods are leading in the diagnosis of diseases of the maxillofacial region, due to their reliability and information content. X-ray diagnostic methods have found wide application in the practice of therapeutic dentistry (for identifying peri- and periodontal diseases); in orthopedic dentistry (to assess the condition of remaining teeth, periapical tissues, periodontal tissue, which determines the choice of orthopedic measures). X-ray methods are also in demand in maxillofacial surgery in the diagnosis of traumatic injuries, inflammatory diseases, cysts, tumors and other pathological conditions. The method and technique of x-ray examination of teeth and jaws has its own characteristics.
The most commonly used in dental practice are:
— plain radiography;
— extraoral radiography of teeth and jaws;
- intraoral radiography.
SURVEY RADIOGRAMS
can be performed in three projections - direct, lateral and anterior semi-axial - and allow you to obtain an image of the entire facial and cerebral skull. The direct projection can be performed with naso-frontal or naso-mental adherence to the cassette. Indications for images in the nasofrontal projection are: injuries and diseases of the brain and facial skull. This installation is also used for sialography and fistulography. Images in the nasomental projection are used: to study the bones of the middle and upper floors of the facial skull, paranasal sinuses. The condition of teeth on radiographs in direct projection is not analyzed.
Lateral photographs of the skull are taken as a mandatory addition to direct ones. However, it is quite difficult to study the condition of the bones of the facial skeleton from these photographs due to the summative effect of the right and left halves of the skull. Usually only gross, extensive bone changes are visible. Lateral photographs are often performed to examine the condition of the skull, its base, sella turcica, sphenoid and frontal sinuses, as well as to determine the location of foreign bodies.
Axial and anterior semi-axial photographs are performed if it is necessary to examine all structures of the base of the skull, bones of the midface, including the orbits, maxillary sinuses, and zygomatic bones.
EXTRAORAL (extraoral)
X-rays of the jaws are taken using both dental and other X-ray machines. X-ray film measuring 13x18 or 18x24 cm and corresponding cassettes with intensifying screens are used. Extraoral radiographs are performed to study the lower jaw, zygomatic bones, temporomandibular joint (TMJ), as well as for sialography and fistulography. Indications for such images may be inflammatory, tumor, traumatic injuries of the jaws, extensive cysts, periodontal lesions of the lower jaw when it is impossible to perform intraoral radiographs. To study the condition of the TMJ, special installations according to Schüller and Parma can be used. Pictures must be taken on both sides to compare the joints.
INTRAORAL radiography
still serves as the basis for radiographic examination in most dental and periodontal diseases. Currently, there are four methods of intraoral radiography used to study the condition of teeth, para- and periodontal tissue:
1. Contact radiography according to the isometric rule.
2. Interproximal radiography.
3. Bitewing radiography (occlusal).
4. Radiography with increasing focal length by a parallel beam of rays (long-focus radiography).
For many years, in the X-ray diagnosis of dental and periodontal diseases, the technique of contact radiography according to the bisector rule or isometric projection, developed by Cieszinski (1907), was mainly used. The main objective of research using this technique is to obtain a clear image of the periapical tissues, therefore the beam is centered on the facial skin at a point corresponding to the projection of the apex of the root of the tooth being studied.
One of the objectives of this technique is to obtain an image of teeth identical to their true size. To reduce projection distortions in practical work, the isometric rule is used - the central beam is directed to the apex of the root of the tooth under study perpendicular to the bisector of the angle formed by the tooth axis and the plane of the film. Any other direction of the central ray leads to lengthening or shortening of the tooth image. It must be remembered that the permissible shortening of the tooth image should not exceed 0.2, and the elongation should not exceed 0.1 of its true dimensions.
However, exact adherence to the isometric rule, unfortunately, is impossible, because It is difficult for each patient to accurately determine the bisector of the angle formed by the axis of the tooth and the plane of the film. Therefore, they use angles of inclination of the tube, calculated empirically for certain groups of teeth. Thus, for images of molars, the angle of inclination of the X-ray tube to the horizontal plane is 25-30°, for premolars - 35°, canines - 45°, incisors - 55°. When photographing the same groups of teeth using the bite technique, the angle increases by 20°.
Equally important is compliance with the orthoradial rule, when using which the central beam at the time of the image is directed perpendicular to the tangent drawn to the dental arch of the upper or lower jaw in the area of the tooth being examined. If this rule is observed, the image of the tooth being examined does not overlap the image of neighboring teeth.
For contact photographs, the film size is 2x3 cm, 3x4 cm (the latter format is available in the form of standard packages), for bite-size photographs the film size is slightly larger - 5x6 cm, 6x8 cm. In the absence of factory packaging, a special film is used for radiography of teeth RM. The corners of the film are cut off so that they do not injure the oral mucosa, and placed in a small envelope made of opaque paper, and then in wax paper. A bag of film is inserted into the oral cavity, and the patient presses it firmly against the hard palate and alveolar process of the area under study with the first finger of the opposite hand. Dental X-rays are usually performed with the patient sitting. The head is fixed on the headrest in the desired position.
When examining the teeth of the upper jaw, the patient's head is placed in a position in which the wings of the nose and the external auditory canal are in a plane parallel to the plane of the floor. The film is inserted into the oral cavity so that its edge is parallel to the occlusal plane and protrudes 0.5 cm from the edge of the teeth, while the tooth to be removed should be in the center of the film. In this position, the film is pressed with the second or first fingers of the patient’s hand to the mucous membrane of the hard palate. The apexes of the roots of the teeth of the upper jaw are usually projected onto the skin of the face along a line connecting the wing of the nose and the tragus of the ear: when examining the central incisors, the beam is directed to the tip of the nose, the lateral incisors to the wing of the nose, and the canines to the upper part of the nasolabial fold.
When radiography of the lower jaw, the patient's head is fixed on the headrest so that the line connecting the angle of the open mouth and the tragus of the ear is in a plane parallel to the floor. To do this, the patient tilts his head back a little. The projection of the apexes of the roots of the teeth of the lower jaw onto the skin of the face corresponds to a line running 1 cm above the lower edge of the jaw. The central beam is directed from bottom to top and medially to the apex of the tooth being examined, while maintaining the angles for the corresponding groups of teeth. When taking photographs using the bite-to-bite technique, the angle increases by 20°.
In some cases, it is necessary to deliberately change the projection of the beam to obtain a separate image of the roots of multi-rooted teeth or to clarify the relationship of the roots with pathological formations. In such cases, oblique intraoral projections are used: mesodistal (the central ray is directed obliquely from the front to the medial and back) and distomedial (the ray is directed from the back to the medial and forward).
Thus, contact radiography according to the isometric rule can be used to obtain images of teeth identical to their true sizes, to obtain a clear image of periapical tissues and to determine the spatial relationships of objects localized in the zone of roots and periapical tissues.
At the same time, the isometric imaging technique has a significant drawback; it does not allow assessing the condition of the marginal sections of the interalveolar ridges, since the latter are filmed with an oblique beam, which leads to a shortening of their image.
That is why it should be abandoned when diagnosing periodontal diseases.
Interproximal radiography is used to obtain a clear, undistorted image of the marginal parts of the alveolar processes of the jaws. The method allows you to objectively assess the degree of bone tissue resorption over time and is the best way to identify proximal and cervical caries.
X-ray film, using special film holders, is placed in the oral cavity parallel to the crowns of the teeth at some distance from them, which makes it possible to obtain an image of symmetrical areas of both jaws. To secure the film, you can use a piece of thick paper attached to the film wrapper and pressed between closed teeth. The central beam is directed perpendicular to the crowns and film. Radiographs simultaneously display the crowns of the teeth and the marginal sections of the alveolar processes of the upper and lower jaws. To study the entire bite, 3-4 photographs are taken.
Bitewing (occlusal) radiography technique. A simple and common technique for intraoral imaging. Bitewing photographs are performed when it is necessary to study large areas of the alveolar process - 4 or more teeth, when looking for impacted and dystopic teeth. Bitewing radiography is used when examining children, as well as in cases where intraoral contact photographs are not possible (in case of jaw damage, TMJ stiffness, increased gag reflex). The technique is indicated for obtaining an image of the floor of the mouth in case of suspected stones of the submandibular and sublingual salivary glands, as well as for studying the condition of the hard palate. Bite X-ray allows you to assess the condition of the outer and inner cortical plates of the jaws in case of cysts and neoplasms, and to identify the reaction of the periosteum.
When conducting occlusal radiography, the rules of bisector and tangent are observed. A film measuring 5x6 or 6x8 cm is inserted between the rows of teeth and is held in place by their closure.
When x-raying the upper jaw, the film is inserted as deep into the oral cavity as possible and clamped between the teeth. The patient sits in a dental chair, the midsagittal plane of the skull is perpendicular to the floor, and the line connecting the tragus of the ear and the wing of the nose should be parallel to the floor of the office. The central beam at an angle of +80° is directed to the root of the nose. The image shows a significant part of the alveolar process of the upper jaw and the floor of the nasal cavity.
When taking pictures of the lower jaw, the patient's head is tilted back so that the line from the corner of the mouth to the tragus of the ear is parallel to the floor of the office. The central beam is directed perpendicular to the film 3-4 cm posterior to the chin. The radiograph clearly shows the area of the floor of the mouth, the buccal and lingual cortical plates of the lower jaw, and the entire dentition in the axial projection.
Long focal radiography (parallel beam imaging) was introduced by Hilscher in 1960 and is increasingly used in many countries instead of contact intraoral radiography. Long-focus radiography allows you to avoid the disadvantages of contact photography and preserve its positive aspects: coverage of a significant part of the alveolar process vertically, a complete image of the tooth, a clear structure of the bone tissue. One of the important advantages of shooting with parallel beams is that the image of the marginal parts of the alveolar processes is not distorted, and therefore the technique can be recommended for wide use in periodontology.
The X-ray film is placed in the mouth parallel to the long axis of the tooth, for which special film holders or hemostatic clamps are used (cotton or gauze rolls can also be used).
For long-focus radiography, devices with a more powerful X-ray tube and a long localizer tube (36-40 cm minimum) are used. The object-film distance ranges from 1.5 to 3 cm, and the central beam hits the film perpendicularly or at an angle of no more than 15°. The image and the object are almost equal in size to each other.
When performing any methods of radiography of the dentofacial apparatus, in order to eliminate dynamic blurriness of the image obtained in the image, an indispensable and most important condition is complete immobility of the patient. For this purpose, it is necessary to ensure the stabilization of the patient using a comfortable chair with a fixing headrest and armrests. Usually the picture is taken 3-4 seconds after the command: “do not breathe.”
In recent years, a new branch of radiation diagnostics has emerged - DIGITAL RADIOGRAPHY
, which is not so much an independent method of x-ray diagnostics as a progressive modification of the transformation of the energy of the x-ray beam. If in classical radiography the radiation receiver was X-ray film, then in digital radiography these are highly sensitive sensors that directly form a digital image (direct digital radiography), or electro-optical converters that create an analog video signal, which is later converted into a digital signal using an analog-to-digital converter signal. The digital code is then processed by a computer and transformed again into a visible (analog) image on the monitor screen. Computer information processing allows you to improve image quality by manipulating contrast, brightness, clarity, size, eliminating technical errors, and highlighting areas of interest. The advantages of digital radiography are also a significant reduction in radiation exposure (tens of times), economic costs (since expensive X-ray film is not used), and the possibility of archiving information. The principle of digital information processing is also used in computer, magnetic resonance imaging and in some modes of ultrasound diagnostics. Currently, digital radiography has become the leading method of radiological diagnostics.
Similar systems are widely used in dental practice: these are X-ray machines, Finnish-made Digora devices, etc. With their help, you can obtain intraoral radiographs and panoramic tomograms.
X-RAY PROTECTION
The widespread use of X-ray examinations in dentistry requires careful monitoring of doses, given that a significant number of patients are children and young people. The biological effect of small doses of ionizing radiation associated with X-ray examinations does not cause immediate radiation reactions, but can cause so-called stochastic long-term consequences in the form of induced malignant diseases, genetic consequences, shortened life span, etc.
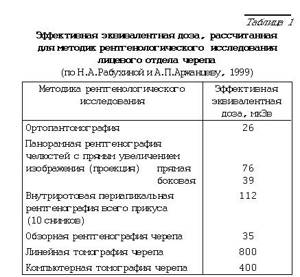
Radiation exposure to patients is assessed using an effective equivalent dose (EDD), which is measured in microsieverts (µSv) and is determined by measuring the exposure of vital organs that are most sensitive to the effects of ionizing radiation (lens of the eye, brain, thyroid gland, etc.).
As can be seen from the table above, the dose loads are especially high when examining the entire dentition, performed on a device of type 5D-1 and 5D-2m without additional protection. Examination using an orthopantomograph sharply reduces the radiation dose to the patient. Additional shielding, including the thyroid gland, makes the study even safer.
Thus. Radiation safety of patients can be ensured in the following ways:
— the dentist’s knowledge of optimal algorithms for examining patients with various types of pathology,
— the dentist’s knowledge of radiation load values using various methods of x-ray examination,
— shielding the patient’s vital and highly sensitive organs,
— diaphragm of the irradiation field,
- reducing research time to a minimum, which is ensured by the quality of the film and intensifying screens.
Special research methods
PANORAMIC RADIOGRAPHY
(Fig. 1) is a technique that allows you to obtain a detailed (slightly enlarged) image of one of the jaws on one film.
Panoramic radiograph of the upper jaw
An X-ray machine with a special high-focus X-ray tube is used to obtain the image. The anode of the X-ray tube is inserted into the patient's mouth during imaging. When photographing the upper dentition, the focus of the tube is placed above the tongue at the level of the fifth teeth; for photographing the lower row, in the area of the frenulum under the tongue.
X-ray film with a format of 18x24 cm is placed in a flexible polyethylene cassette with high-resolution intensifying screens. During filming, the patient presses the cassette with his hands to the skin around the area of the face being examined. If the cassette is not firmly fixed, the image of the bone structure will be unclear.
Since the focus of the X-ray tube is as close as possible to the object of study, and the film is located at a certain distance from the teeth, due to the thickness of the soft tissues, the image is almost doubled in size. Thanks to this circumstance, small details that are poorly visible on conventional x-rays are visible in panoramic images.
Panoramic photographs of the upper jaw also provide images of the maxillary sinuses, nasal cavity, cusps of the upper jaw and zygomatic bones. The inferior panoramic radiograph clearly shows the mandibular canal and the base of the mandibular bone. The lateral panoramic image simultaneously displays the teeth of the upper and lower rows of each half of the jaw.
Based on panoramic images, caries and its complications, inflammatory processes, cysts, neoplasms and traumatic injuries of the jaws are diagnosed. However, this method is not suitable for assessing the degree of resorption of interalveolar ridges.
Another disadvantage of panoramic radiography is the inability to control the position of the X-ray tube applicator in the mouth.
This research method exposes the oral mucosa to significant radiation, so panoramic radiography is recommended to be used only when indicated and no more than 1-2 times a year for each patient. Additional protection with this type of radiography is ineffective, because Oral organs located outside the protective zone are exposed to irradiation.
It should be borne in mind that this technique, due to the emergence in recent years of more modern research methods, is rarely used.
LINEAR TOMOGRAPHY or layer-by-layer radiography
– a method that allows you to eliminate the summative nature of the image and most clearly highlight a certain flat layer of the organ or area being studied. The essence of the method is the synchronous movement of the tube and film relative to the patient. A clear image of the layer located at the level of the geometric axis of rotation of the lever is obtained. The remaining elements of the object are blurred as a result of the dynamic blur effect. The swing angle of the X-ray tube during tomography is 30-60 є, the slice thickness is 0.2-0.5 cm. Typically, tomography is performed after survey X-rays have been taken, which make it possible to determine the required slice depth.
In dentistry, tomography is used to study the TMJ, for complex fractures of the midface, post-traumatic deformities, neoplasms, inflammatory processes and can be performed in direct and lateral projections. In the last 10-15 years, LINEAR ZONOGRAPHY has been widely used in practice - layer-by-layer research with a small swing angle of the X-ray tube (usually 8º). The advantage of zonography is that it produces thicker slices, which reduces the number of images, makes the procedure more economical and safe in terms of radiation exposure, and obtains the same information as a series of tomograms.
ORTHOPANTOMOGRAPHY (panoramic tomography)
– a method that allows you to obtain an image of a curved layer on a flat X-ray film. During shooting, the tube and film cassette describe an incomplete circle around the patient’s head (270º). At the same time, the cassette rotates around its own vertical axis, as if “rolling” the patient’s jaws from the front. The X-ray beam passes through a 2 mm wide slit-shaped diaphragm, then through the anatomical structures of the head and facial part of the skull and enters new unexposed areas of the film. As with linear tomography, anatomical structures distant from the film are projectedly enlarged and their image is blurred. Modern orthopantomographs provide programs for studying the dentition, the bone structure of the upper, middle and lower zones of the facial skull, the TMJ, as well as the craniovertebral junction, the inner and middle ear, and the optic nerve canal. It is possible to change the thickness and depth of the layer being studied.
Panoramic tomogram of the lower face area
The simplicity of the method, high information content and relatively low radiation exposure allow the technique to be widely used for diagnosing almost the entire range of diseases of the maxillofacial area.
The disadvantages of the method include the unequal degree of magnification of the resulting image, as well as the deformation of anatomical structures in some types of devices.
PANORAMIC ZONOGRAPHY method
is a type of orthopantomography that allows you to obtain an image of a thicker layer of the object (up to 3 cm), which increases the information content of the method.
Panoramic zonogram of the midface
TELERENTGRAPHY
– a technique that allows you to obtain images of anatomical structures with minimal projection magnification. During teleradiography, the object of study and the film cassette are moved away from the X-ray tube to a distance of 2-2.5 m or more. The image magnification is 2-4% and can practically be neglected. Teleradiograms of the skull are performed on films measuring 24x30 cm. The photographs should show not only bone structures, but also soft tissues of the maxillofacial area, soft palate, tongue, and posterior wall of the pharynx. If necessary, soft tissues are marked with a viscous contrast agent (iodolipol, bariodol, etc.), and radiopaque marks are also applied to the soft palate. Subsequently, craniometric calculations are performed according to a certain scheme. Despite the errors that arise when analyzing teleroentgenograms, the technique is widely used in orthodontics for diagnosing and planning the treatment of malocclusions, as well as for planning surgical treatment for congenital and acquired deformities of the maxillofacial region.
CT SCAN
allows you to obtain a cross-sectional layer-by-layer image of any area of the human body, including the skull. It is based on recording the energy of a beam of X-ray radiation passing through the human body at different angles when the tube is rotated by highly sensitive sensors that convert the received information into electrical signals. The latter are “digitized” and sent for analysis to a computer, where the program allows you to calculate the density of each voxel (volume unit of the layer) and present it on the display screen in the form of a pixel of the corresponding brightness. Contrast enhancement techniques are used to enhance tissue contrast. A series of cross sections can be transformed into a planar or volumetric image in any longitudinal plane.
The examination is not burdensome for the patient; when examining the maxillofacial area, it does not require special preparation.
CT is used in the diagnosis of diseases of the facial skull and dental system: fractures, tumors, cysts, systemic diseases, pathology of the salivary glands and TMJ. CT examination is especially indicated for processes in hard-to-reach locations (ethmoidal labyrinth, sphenoid bone, pterygopalatine fossa, etc.). Spiral CT scanners have a new “dental” program for studying the dentition.
However, the use of this method is associated with significant radiation exposure to the patient. Thus, with CT of the facial skull, the surface dose is 2-10, and the dose to the lens of the eye is 100 times higher than that with radiography and linear tomography.
MAGNETIC RESONANCE TOMOGRAPHY (MRI)
- a method of radiation diagnostics based on recording the energy emitted by protons of hydrogen nuclei in the internal environments of the human body when they return from an excited state to their original state (so-called relaxation). Resonant excitation of nuclei and the spin effect occur under the influence of radio frequency pulses generated by the interaction of a magnet creating a static magnetic field and an additional high-frequency coil. The latter also serves to record the relaxation signal. A powerful computer analyzes the information received.
MRI allows you to obtain images of the layers of the human body in any plane - frontal, sagittal, axial, etc., which can then be reconstructed into three-dimensional images.
To enhance the contrast of the tissues being studied, chemical substances containing nuclei with an odd number of protons and neutrons (fluorine compounds, paramagnetic substances) are used, which change the relaxation time of water. This method has advantages in visualizing soft tissues, such as muscle, fat, cartilage, etc., which makes its use especially necessary when studying the TMJ, mucous membranes of the paranasal sinuses and oral cavity, salivary glands and other soft tissue structures of the head and neck . The method is not burdensome for the patient and does not have any harmful effects on his body. A contraindication for MRI examination is the presence of metal foreign bodies in the patient (including some types of crowns). Artificial contrast techniques
Artificial contrast is widely used in practical work in the study of: ducts of the salivary glands (sialography), fistulous tracts (fistulography), maxillary sinuses (maxillary sinusography), etc.
SIALOGRAPHY.
On plain radiographs, the salivary glands are usually not visible; only shadows of radiopaque salivary stones can be detected. To examine the ducts of the salivary glands, 1.5-3 ml of contrast agent is injected at the mouth of the duct using a blunt-tipped needle or through a thin catheter until a feeling of tension appears in the gland area. As contrast agents, water-soluble contrast agents of high viscosity or sharply diluted and emulsified oil preparations (dianosyl, ultra-liquid lipiodol, ethiodol, mayodil, etc.) are used. Pictures are taken in frontal and lateral projections. To obtain a contrast image of all major salivary glands simultaneously, orthopantomography is also indicated. Sialography is used to diagnose salivary stone disease, inflammatory and tumor processes.
DOUBLE CONTRAST
– the technique consists of simultaneous injection of lipoiodol into the ducts of the salivary glands, and oxygen into the tissues surrounding the gland. This technique is the most informative in the diagnosis of tumor processes of the salivary glands.
FISTULOGRAPHY
– filling the fistula tracts with a contrast agent in order to study their extent, direction, and connection with the pathological process in the image. Warmed iodolipol is used as a contrast agent. Immediately after the administration of the contrast agent, photographs are taken in two mutually perpendicular projections.
ARTHROGRAPHY
used to study the condition of the TMJ and, first of all, to clarify the condition of the intra-articular meniscus. Under the control of a television screen, 0.8-1.5 ml of a viscous water-soluble contrast agent is injected into the joint cavity and tomograms or zonograms of the joint are performed with the mouth open and closed.
ANGIOGRAPHY
– a technique for studying the vessels of the maxillofacial area using water-soluble and non-ionic contrast agents (cardiotrast, verografin, hypaque, omnipaque, ultravist, etc.). The technique is performed in a cath lab environment.
Angiography is used to diagnose diseases and anomalies of the vascular system (hemangiomas, juvenile angiofibromas of the skull base). In the practice of maxillofacial surgery, this technique is used quite rarely.
HIMOROGRAPHY
– X-ray examination of the maxillary sinuses after introducing a contrast agent into them by puncturing its wall, through the socket of an extracted tooth (if there is communication with the sinus) or through a fistulous tract. After aspiration of the sinus contents, 3-7 ml of slightly warmed contrast (iodolipol, iodipine, lipiodol, etc.) is injected. Pictures are taken in the nasomental and lateral projections. The technique is indicated for the diagnosis of cysts, sinus polyps, productive forms of sinusitis, and tumor diseases.
ULTRASONOGRAPHY.
The method is based on the effect of registering reflected ultrasonic radiation within the range of 1.0-2.0 MHz and forming a linear (static) or multidimensional (dynamic) image. The method is harmless and informative when studying soft tissues. It is quite widely used in the diagnosis of diseases of the salivary glands, pathology of the soft tissues of the neck, and lymph nodes.
Source:
I.I. Sergeeva, T.F. Tikhomirov, V.V. Rozhkovskaya, N.A. Savrasova
Belarusian State Medical University
based on materials from zhuravlev.info
Computed tomogram is the most informative x-ray examination
Just as the advent of X-rays revolutionized diagnostics, the capabilities of computed tomography (CT) have taken diagnosis and treatment to a whole new level.
By passing X-rays from different angles, using highly sensitive detectors and sophisticated software, computer tomographs can create three-dimensional models of any elements of the dental system.
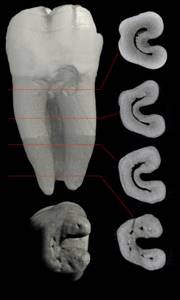
On a tomogram, you can zoom in on any object for a closer look; get a slice of the image to see the “extra” channel; assess the quality of filling along the entire length of the canal; detect cracked teeth; identify foci of chronic infection that are “hidden” due to their size or location.
A CT scan is necessary to plan many types of dental treatment.
For example, before starting prosthetics on implants, a tomogram allows you to assess the density and amount of bone tissue, select the optimal size of implants, installation sites and angle of inclination.
Sometimes the photo needs to be repeated
X-ray images are needed not only at the diagnostic stage and for monitoring during treatment, but also in the process of monitoring the results of treatment.
For example, after endodontic treatment of chronic foci of infection or “deep” caries, the doctor may order a repeat X-ray examination. This is due to the relative unpredictability of treatment results and the desire to avoid possible complications.
Read about the difficulties of endodontic treatment in the articles:
- Why are granulomas and dental cysts dangerous for your health?
- Why can’t we give a 100% guarantee on root canal treatment?
Optimal choice of radiation diagnostic methods
1. When referring patients to these diagnostic methods, attending physicians must take into account the diagnostic effectiveness of each method when examining various organs and systems and the indications for their use. (If it is difficult to choose the most informative diagnostic method, consultation with specialists from CT/MRI rooms is recommended.)
2. All studies are carried out strictly in the presence of clinical indications, or in case of questionable data from other methods (ultrasound, CT, MRI, scintigraphy, etc.), preparation for surgical interventions, monitoring of treatment (including response to chemotherapy).
3. The final decision to conduct the study is made by the radiologist in the CT/MRI room, who also determines the necessary methods and scope of the study (including the study using contrast agents). 4. When conducting intravascular contrast studies using radiopaque agents, it is mandatory to fill out the patient’s informed consent
for the study in the established form.
Currently, the following radiation diagnostic methods are used in medical institutions:
1. X-ray diagnostics traditional
(radiography, fluoroscopy).
The method is based on recording X-ray radiation passing through the patient's body in one projection. 2. X-ray computed tomography
(MSCT/CT).
The method is based on obtaining layer-by-layer images in an axial projection with further three-dimensional and multiplanar reconstructions. 3. Magnetic resonance imaging
(MRI).
The method for obtaining layer-by-layer and volumetric images is based on the phenomenon of nuclear magnetic resonance. 4. Ultrasound diagnostics
(USD). The method of obtaining layer-by-layer images is based on the study of the reflection of ultrasonic waves from tissues.
Based on their ability to cause tissue ionization, radiation diagnostic methods are divided into ionizing (CT, X-ray and radionuclide studies) and non-ionizing (ultrasound, MRI).
When choosing one or another diagnostic method to solve a specific clinical problem, the doctor must rely on the following criteria:
1. Information content of the method. Diagnostics should not go from simple to complex; it is necessary to immediately select the most informative methods. 2. Harmful to the patient. In all cases of using X-ray (ionizing) or invasive research there must be a serious justification. X-ray examination should be replaced by radiation-safe ultrasound in cases of comparability of methods. 3. Economic costs. The value of a method is directly proportional to its informativeness and inversely proportional to harm and cost. The use of expensive MRI and MSCT technologies is justified only with strict clinical justification. 4. Availability of the method.
Diseases of the central nervous system
Radiation diagnostics of pathology of the spine and spinal cord
The spine is initially examined using radiography (standard spondylography in two projections). If it is necessary to clarify the natural mobility in the spinal segments, functional photographs are taken.
Contraindications for functional tests are:
· Neurological deficit (motor and sensory disorders).
· Bone injuries: In the diagnosis of pathology of the cervical spine with the presence of cerebral symptoms or pyramidal disorders, it is necessary to study the blood flow of the arteries of the head in the neck area - duplex ultrasound and MR angiography.
To determine the type and magnitude of spinal deformity, spondylography is performed. MRI is recommended if myelopathy is suspected. In the diagnosis of degenerative diseases (osteochondrosis, spondylosis, spondylarthrosis), the main imaging method is radiography. CT and MRI should not be used to diagnose this pathology. MRI is the “gold standard” for examining intervertebral discs and is used in the diagnosis of intervertebral disc herniations. In the lumbar region, it is permissible (if MRI is not possible) to use CT to detect hernias. In the cervical and thoracic regions, the use of CT to detect intervertebral disc herniation is not indicated due to low information content. MRI is the method of choice in the differential diagnosis of postoperative fibrous changes from hernia recurrence, and the use of contrast increases accuracy. CT/MRI – methods for diagnosing spinal canal stenosis. The method of choice for studying ligaments, nerve roots, and structures of the spinal canal is MRI. MRI is the “gold standard” for diagnosing spinal cord lesions of any origin. CT is not used for a survey of the spine. CT is prescribed strictly taking into account the localization of changes in a limited number of segments of the spine and changes in the paravertebral soft tissues of the area under study. In the diagnosis of spinal tumors, when changes suspicious for a tumor are detected on spondylograms, CT and MRI are used to clarify the identified lesion and staging the tumor. In the diagnosis of inflammatory diseases
(specific and nonspecific spondylitis) of the spine requires a comprehensive radiation examination: radiography, CT, MRI, taking into account the information content and indications for each method depending on the stage and location of the disease.
In the diagnosis of tuberculous spondylitis
(spondylitis of other etiology) requires the comprehensive use of radiation methods. Initially, radiography and MRI should be performed.
Traditional X-ray tomographic methods are effective in the advanced stage of the disease. MRI is informative already in the early phases of spondylitis and is the method of choice for identifying the causes of neurological disorders. CT is used additionally after radiography and MRI as a method to clarify the nature of pathological changes.
CT and MRI are not competing methods, but complementary.
CT can be used as a primary method for diagnosing brain lesions.
Intravenous contrast increases diagnostic accuracy. MRI is primarily recommended for identifying changes in the posterior cranial fossa, brainstem and midline structures in the presence of corresponding neurological symptoms. CT is more informative for diagnosing bone lesions of the skull, intracranial calcifications, and fresh intracranial hemorrhage.
Traumatic brain injury (TBI)
Patients with traumatic brain injury are first treated with CT as the most effective method for diagnosing damage to the bone structures of the base of the skull, the brain, its membranes and blood vessels. In case of severe TBI, CT is performed according to urgent indications.
Indications for CT scan for TBI:
1. Presence of focal neurological symptoms. 2. Impaired consciousness. 3. Penetrating damage. 4. Depressed skull fractures. 5. Detection of blood during lumbar puncture. 6. Increasing symptoms in the first days after injury. 7. Mechanism of injury characteristic of brain damage.
MRI
used in the diagnosis of brain contusions, subacute and chronic hemorrhages (from the 3rd day and later after injury), diffuse axonal damage (DAI). MRI is the most informative method for visualizing cerebral edema, DAP in patients in a coma. Traditional craniography is informative in diagnosing calvarial fractures. X-ray may not be performed after a CT scan that reveals bone lesions or indications for emergency surgery.
Brain tumors
None of the radiodiagnostic methods is comprehensive for diagnosing a tumor. As a rule, a comprehensive study is required - CT and MRI. To increase the information content of the study and differential diagnosis, contrast enhancement with iodine-containing or paramagnetic contrast agent is required. Establishing the probable histological structure of a tumor by tomographic methods is not always possible. In the diagnosis of tumors of the posterior cranial fossa and pituitary gland, MRI is primarily recommended. MRI with contrast is recommended for postoperative monitoring of the radicality of tumor removal.
Metastases in the brain
MRI and CT with contrast are informative in the diagnosis of metastases. When identifying a single volumetric formation suspicious for metastasis, in the absence of evidence of a primary malignant tumor, a comprehensive examination is required aimed at searching for the primary tumor.
Tumors of the cranial nerves
The method of choice for suspected neuroma is MRI. MRI visualizes the auditory nerves (VII-VIII are not differentiated separately) and, not always, the trigeminal nerves (V pair). To identify destruction of the temporal bone pyramid, an additional CT scan is used.
Vascular diseases
In acute cerebrovascular accidents (ACI) of any type, CT is primarily indicated (differential diagnosis of hemorrhagic and ischemic stroke). This is important, because for stroke of ischemic and hemorrhagic types, treatment is different. CT reveals minimal hemorrhages immediately after formation, therefore, with the clinical picture of stroke and the absence of changes on tomograms characteristic of a hemorrhagic stroke, an ischemic stroke (IS) is assumed. MRI is more sensitive in diagnosing ischemic brain lesions, regardless of the stage of the disease. MRI is the method of choice for identifying brainstem, small lacunar infarcts and ischemic foci localized in the posterior cranial fossa (less easily identified by CT). The use of CT or MRI depends on the moment of stroke onset, i.e. The timing of detection of ischemic brain damage is of paramount importance for the choice of imaging method. In the acute stage of development of ischemic stroke (up to 6 hours), damage to brain tissue cannot be determined on native CT. During this period, in order to clarify the diagnosis of ischemic stroke and differentiate zones of irreversible/reversible damage to brain tissue, perfusion CT is necessary (in the absence of CT signs of hemorrhagic stroke). In addition, perfusion CT allows one to determine the degree of reduction in cerebral blood flow during ischemic stroke. If perfusion CT is not possible, MRI with diffusion assessment (MRI-DWI) and the state of intracranial arteries (MRA) is indicated. On the first day of the disease, MRI-DWI is more informative than native CT. In the period from the beginning of the second day to 8 days from the onset of the disease, both CT and MRI are informative. Repeated CT/MRI is not used to monitor the course of the disease during treatment. However, CT is recommended for diagnosing complications of stroke (mass impact, secondary hemorrhage, development of hydrocephalus).
If acute intracranial hemorrhage is suspected, CT is initially indicated
The detection rate of subarachnoid hemorrhage (SAH) on CT is greatest in the first day, then it constantly decreases and after 1-2 weeks, signs of hemorrhage are practically undetectable. CT angiography significantly improves the effectiveness of identifying the location and cause of non-traumatic hemorrhage, but the presence of hemorrhage makes the detection of small arterial aneurysms difficult. MRI diagnosis of intracerebral and subarachnoid hemorrhages in the first day is difficult. In the subacute (3-14 days) and chronic stages (more than 14 days), MRI is highly informative.
In the diagnosis of variants and malformations of cerebral vessels
, incl. arterial aneurysms and vascular malformations - MRI in combination with MR angiography is primarily recommended. CT angiography is a method of clarifying diagnosis, especially with inconclusive MRI data. In doubtful cases and when planning surgical treatment, cerebral angiography is performed. To study extracranial vessels (branches of the aortic arch), duplex ultrasound examination is primarily used. Specifying methods for identified pathological changes are MRA and CTA.
Inflammatory diseases (abscess, meningitis) - MRI or CT with contrast
Viral infections
(encephalitis) MRI is the method of choice.
Parasitic infections of the brain
- CT scan.
If a parasitic lesion of the brain is suspected, an additional CT examination of the chest and abdominal cavity (diagnosis of the lungs and liver) is necessary. Demyelinating diseases
(multiple sclerosis, etc.) MRI – method of choice + contrast
Epilepsy
– MRI and/or CT.
Hydrocephalus
- MRI or CT
Degenerative and metabolic diseases
- MRI and CT.
Diseases of the head and neck Diseases of the paranasal sinuses.
For visualization of the paranasal sinuses, the primary method is radiography. In case of chronic atypical sinusitis, as well as when endoscopic examination is impossible, CT is used to clarify the nature of the identified changes and differential diagnosis. MRI for clarifying diagnostics.
Indications for CT
· Chronic atypical rhinosinusitis. · Diagnosis of sinus development options. · Determination of the prevalence of the pathological process. · Assessment of the condition of deep soft tissue structures. · Complications of rhinosinusitis (subperiosteal abscess, osteomyelitis of the skull bones, etc.). · Polyps and polyposis of the nasal cavity and paranasal sinuses. · Wegener's granulomatosis. · Tumors of the paranasal sinuses. · Planning of surgical and/or radiation treatment.
Indications for MRI
· To identify intracranial and intraorbital complications and spread of sinusitis. · In the differential diagnosis of a fungal process from inflammation of another etiology. · Complements CT in complex diagnosis and assessment of the prevalence of tumors.
Eye diseases
Ultrasound, CT and MRI are used in the diagnosis of diseases and injuries of the eye and orbit. Ultrasound and MRI are the methods of choice for detecting retinal detachment. In addition, ultrasound is used in the diagnosis of hemophthalmos and intraorbital foreign bodies. CT and MRI are indicated in the diagnosis of tumors and inflammatory processes. CT complements MRI in identifying calcifications and bone destructive changes. MRI is used to diagnose non-metallic foreign bodies of the eye, subacute and chronic hemorrhages (8-21 days). MRI is contraindicated for metallic foreign bodies in the orbit.
Main indications for CT and MRI
· Vascular tumors of the orbit - CT scan with contrast. MRI for clarification. · Dermoid and epidermoid of the orbit - CT. MRI for clarification. · Idiopathic pseudotumor of the orbit - MRI. · Tumors of the optic nerve - MRI. CT scan for clarification. · Optic neuritis is the method of choice for MRI. · Melanoma of the eyeball – primary ultrasound. MRI for clarification. · Retinoblastoma – complex MRI/CT examination. · Tumors of the lacrimal gland - CT. MRI for staging a malignant tumor. · Lymphoproliferative diseases of the orbit - MRI. · Orbital abscess - MRI, especially if intracerebral complications are suspected (MRI), CT to assess bone changes in the walls of the orbit. · Eye trauma – CT is the method of choice: determining damage to the walls of the orbit, identifying foreign bodies, acute intraorbital hemorrhages.
Diseases of the soft tissues of the neck
Ultrasound is the primary method for visualizing cysts, inflammatory changes and lymph nodes (including non-palpable ones). If ultrasound data is inconclusive, CT is indicated. MRI with contrast is the method of choice for identifying and assessing the extent of the tumor process. CT with contrast if MRI is not possible.
Ear diseases
For developmental anomalies and diseases of the middle and inner ear, the method of choice is CT. Special radiographic placements according to Schuler, Mayer, Stenvers, if CT is possible, are of secondary information content. If a temporal bone fracture is suspected, the method of choice is CT. MRI is also indicated for diagnosing intracranial complications of middle ear diseases. MRI is recommended to identify lesions of the vestibulocochlear nerves in patients with sensorineural hearing loss.
Diseases of the pharynx and larynx
To clarify the extent of the tumor or inflammatory process, evaluate regional lymph nodes and obtain additional information, MRI or CT scan with contrast. In the radiological diagnosis of diseases of the larynx, it is initially recommended to perform a lateral radiograph of the neck and linear tomography of the larynx. This technique is quite informative, especially for diagnosing subglottic stenosis of the larynx and tracheal stenosis.
Inflammatory diseases of the jaws
Radiation diagnosis of osteomyelitis depends on the stage. In the acute stage, the x-ray picture is negative. Ultrasound during this period may reveal accumulation of pus under the periosteum and in soft tissues. The first radiological signs appear 10-14 days after the onset of the disease. In the subacute and chronic stages, radiographic examinations and, if necessary, CT scans are performed.
Neoplasms of the jaws
In the diagnosis of odontogenic and non-odontogenic cysts and benign tumors, radiographs are primarily indicated; if necessary, CT is additionally used.
Hemangioma
(in soft tissues or inside bone) is detected radiographically, CT and CTA are used to determine its extent. Radiography is the main method for diagnosing fibrous dysplasia.
Malignant tumors (cancer, sarcoma, metastases)
– the main methods are radiography and CT. MRI allows you to detect cancer of the mucous membrane of the maxillary sinus at an early stage (before the onset of bone destruction) and at a late stage complements CT in assessing the extent of the process. In the diagnosis of relapses, a comprehensive X-ray examination is used: radiography, CT and MRI.
Diseases of the salivary glands
Radiation diagnosis of diseases of the salivary glands is based on the use of ultrasound (primarily) and sialography. In case of complications and suspicion of a malignant lesion, MRI is used.
Disorders of the temporomandibular joint (TMJ)
In the radiological diagnosis of TMJ diseases (arthrosis deformans, arthritis), radiography, CT and MRI are used. MRI is the method of choice in the diagnosis of functional disorders of the TMJ.
Injuries of the maxillofacial area (MFA)
1. Patients with isolated injuries of the facial skeleton are shown radiography in standard and/or special settings. 2. To search for radiopaque (metal-containing) foreign bodies of the maxillofacial area, radiography is primarily indicated. 3. CT is the method of choice to clarify the localization of a foreign body in relation to the orbital structures. 4. CT is indicated in cases of intracranial foreign bodies. 5. CT is the method of choice for multiple and combined trauma and complex cases. 6. CT is indicated for gunshot and blast injuries of the facial skeleton. 7. CT is indicated when choosing treatment tactics and planning plastic surgery.
Smirnov V.V.
.
— Ph.D., doctor of the highest qualification category. Savvova M.V.
- doctor of the highest qualification category.