“The results of an ultrasound of the mammary glands revealed a formation suspicious for oncology,” “the results of mammography do not clearly exclude the presence of a malignant formation,” “a biopsy showed the presence of cancerous changes in the mammary gland and an extensive examination is required.” These are just a few of the worst words a woman can hear from her doctor.
The mammary glands consist of three main types of tissue - adipose, connective and glandular. Breast cancer (BC) is a malignant tumor of the mammary gland that develops from glandular tissue cells. Contrary to popular belief, breast cancer affects both women and men, but it is approximately 100 times more common in women.
- How does breast cancer occur?
- Types of Breast Cancer
- Causes and risk factors
- Symptoms
- Self-diagnosis
- Diagnosis by an oncologist-mammologist
- Stages of breast cancer
- Breast cancer treatment
- Prognosis for breast cancer
How does breast cancer occur?
Breast cancer develops in the same way as any other malignant tumor. One or more cells of glandular tissue, as a result of a mutation that has occurred in them, begin to divide abnormally quickly. They form a tumor that can grow into neighboring tissues and create secondary tumor foci - metastases.
Mutations that lead to breast cancer can be hereditary or acquired.
Common hereditary genetic causes are mutations in the BRCA1 and BRCA2 genes. BRCA1 mutation carriers have a 55–65% risk of developing breast cancer, and BRCA2 carriers have a 45% risk of developing breast cancer. Such genetic defects are inherited from parents to children and cause cancer in approximately 15% of cases.
Much more often, breast cancer occurs due to acquired mutations: they arise in the cells of the gland and are not inherited. For example, in 20% of cases, the number of copies of the gene encoding HER2, a receptor protein that is located on the surface of cells and stimulates their reproduction, is increased.
The “molecular genetic portrait” of a breast tumor is important when choosing the optimal treatment.
When to be examined after breast cancer surgery
If you have not undergone a full examination before starting treatment, go through it at least during the treatment process : of course, some things may no longer be noticed (became invisible during treatment), but at least you will have the results of correct examinations with which you can will compare subsequent ones, and if something is revealed, then we will at least have a clear understanding of the true state of your illness and (if necessary) adjust further treatment.
| For more information about how you should be examined before surgery, see HERE |
It is advisable to carry out the first examination 6 months after completion of chemotherapy and/or radiation therapy : it is unlikely that metastases will grow during treatment with these methods: they are quite effective. Then perform them in the rhythm indicated below.
Types of Breast Cancer
Types of breast cancer are divided into two groups: ductal and glandular. Ductal cancer is more common. It can be intraepithelial (in situ) and invasive. Intracellular ductal breast cancer has a more favorable prognosis, it rarely metastasizes and is curable in 98% of cases. The invasive version of the tumor is prone to uncontrolled growth and generalization of the process.
Glandular cancer can be lobular (invasive lobular carcinoma) or grow from other cells of the glandular tissue. Lobular cancer is often characterized by multicentric growth. The rate of increase in size and timing of metastasis of forms of nodular breast cancer depend on the degree of differentiation of the breast tumor.
Causes and risk factors
Unfortunately, scientists do not yet have complete information about the causes of breast cancer. There is a list of risk factors that affect the likelihood of cancer, but some people are diagnosed with the disease in the absence of these factors, while others remain healthy even if many of them are present. Nevertheless, scientists still associate the occurrence of malignant breast tumors with certain circumstances that most often precede its appearance. These include:
- Age. The majority of breast cancer cases occur in women aged 55 years and older.
- Heredity. If breast cancer is diagnosed in one of your close relatives, the risk doubles.
- History of breast cancer.
- Increased breast tissue density as determined by mammography.
- Some benign neoplasms in the mammary gland.
- Early onset of menstruation - before 12 years of age.
- Late menopause - after 55 years.
- Lack of children or late (after 35 years) first birth.
- Exposure to radiation, such as from radiation therapy given to treat another type of cancer.
- Smoking and drinking alcohol. If a woman consumes 28–42 g of ethyl alcohol daily, her risks increase by 20%.
- Excess weight and low physical activity.
- Use of hormonal drugs: oral contraceptives, hormone replacement therapy in postmenopause.
- Breast injuries.
- Diabetes.
- Work on a schedule with night shifts.

Is it possible for patients to have fluorography and mammography on the same day?
It is a controversial question whether it is possible to do fluorography and mammography on the same day. When prescribing procedures, the urgent need for these diagnostics is taken into account.
Mammography: contraindications and what pathologies it reveals
Mammography is a non-invasive research method during which the breast is placed between special plates to diagnose the condition of the mammary glands.
Due to the fact that scanning is performed using x-ray radiation, mammography has a number of contraindications. Diagnostics is prohibited:
- during pregnancy;
- during breastfeeding;
- if the skin of the breast is damaged.
Relative contraindications include:
- age up to 35 years;
- breast implants.
If the patient has had breast enlargement, the doctor who prescribes mammography must be informed about this. Implants interfere with the normal breast scanning process. For this reason, diagnostics may be inconclusive.
Scanning breast tissue can reveal the following pathologies:
- Cysts. The neoplasm forms in the ducts. The inside is filled with liquid. X-ray examination identifies the cyst as a tumor, so additional examination is necessary.
- Mastopathy. Fibrocystic disease is characterized by the proliferation of pathological tissues. Mammography allows you to identify pathology at an early stage, when there are still no symptoms of the disease.
- Fibroadenoma. Benign tumor.
- Malignant neoplasms. Mammography allows you to diagnose cancer in its early stages.
When performing digital mammography with tomosynthesis, it is possible to identify pathological areas that are not determined by palpation or visually. The effectiveness of diagnosis is due to the fact that the examination of the mammary glands is carried out using successive tomograms produced at a given depth with a fixed distance between slices.
Fluorography: contraindications and what it reveals
Fluorography is a procedure that is performed to identify pathologies of the chest organs. The study is carried out using x-rays.
The device photographs tissues and organs, and then records the image on a special film or displays it on a monitor. Some time after the session, a specialist radiologist deciphers the results.
Fluorography can reveal:
- pneumonia;
- traces of the tuberculosis process;
- fibrosis;
- fluid in the pleural cavity;
- pneumothorax;
- pathological enlargement of the lungs or heart;
- infiltrates;
- organ displacement;
- oncological neoplasms;
- hypertrophy.
The study cannot be carried out during pregnancy and breastfeeding. A contraindication to fluorography is shortness of breath or other severe condition in which the patient cannot hold his breath. Fluorography is also not recommended for children under 15 years of age.
Is it possible to complete them in one day and in what cases is this possible?
Mammography and fluorography can be performed simultaneously, but only on the recommendation of a doctor. Both diagnostics are carried out using x-rays. The radiation dose for each of these procedures is safe for the patient, but if mammography and fluorography are performed simultaneously, the amount of radiation doubles.
A one-time examination of the mammary glands and chest organs on day 1 will not cause the development of radiation sickness, but the immune system is depleted.
If diagnostics are carried out routinely or for preventive purposes, combining them is not recommended.
The indication for mammography and fluorography on day 1 is suspicion of breast cancer or another disease.
How often can each procedure be done?
How long after a repeat scan can be done is determined by a mammologist or radiologist. According to standards, the interval between radiation examinations should be at least 3 months.
For preventive purposes, it is recommended to undergo fluorography once a year. There are professions that require research once every 6 months. The need for additional medical diagnostics arises due to the increased risk of developing diseases with subsequent infection of others.
After 35 years of age, mammography should be performed at least once every 2 years. If a patient experiences changes in the structure of the mammary glands (not dangerous), then diagnostics are prescribed once every six months. It allows you to track the dynamics of the development of pathology. Mammography may be performed more often, for example, to evaluate the effectiveness of a therapeutic course.
To reduce the dose of radiation, the examination should be performed using modern digital tomographs. On these devices, the dosage is 3 times less than in film devices.
Source: https://iDiagnost.ru/issledovaniya/fluorografiya/mozhno-li-patsientam-delat-v-odin-den-flyuorografiyu-i-mammografiyu
Symptoms
In the early stages, breast cancer usually does not manifest itself in any way. Most often, the tumor is discovered by the patients themselves or is detected accidentally during preventive studies.
Patients usually complain of the presence of a palpable formation and discharge from the nipple. Pain is a rare symptom of breast cancer, but pain syndrome can come to the fore at the stage of generalization of the process, especially when metastases spread to the bones.
Quite often, signs of breast cancer are detected, such as the appearance of asymmetry due to changes in the size of the affected gland. Reduction, upward displacement, deformation and wrinkling of the mammary gland can be observed in the scirrhous (fibrous) form of breast cancer. On the contrary, the breast on the affected side becomes enlarged due to the rapid growth of the formation or due to edema, which forms due to impaired lymph outflow.
When the tumor spreads into the subcutaneous tissue, skin changes may be observed. In this case, the following symptoms are revealed:
- “Platform” - the skin above the tumor becomes flattened; it is impossible to form a skin fold in this area.
- “Umbilization” - the skin of the mammary gland over the site of the lesion is wrinkled and retracted.
- “Lemon peel” is a characteristic appearance of the mammary gland due to lymphostasis.
Sometimes, when cancer spreads to the surface of the skin, signs such as redness and ulceration may be observed. The presence of these symptoms indicates that the process is neglected.
Changes in the nipple can also be detected, but only in the later stages. In this case, symptoms such as:
- Forga's sign - on the affected side the nipple is higher than on the healthy breast.
- Krause's sign - the nipple is thickened, the folds of the areola are noticeably pronounced.
Pathological discharge is a rather rare symptom, but in some cases it may be the only one detected during examination. The discharge is often bloody in nature, serous and purulent are less common.
Depending on the manifestations of the disease, different clinical forms of breast cancer are distinguished. In 75–80% of cases, the nodular form occurs. In the early stages, the only symptom is usually a painless lump in the breast. If you divide the breast into four parts by horizontal and vertical lines, then in half of the cases the tumor will be located in the upper outer part.
There are special forms of breast cancer with typical symptoms. These include:
- An edematous-infiltrative form, which is characterized by enlargement and swelling of the mammary gland, marbled skin color, and severe hyperemia.
- Mastitis-like is manifested by thickening of the affected mammary gland, increased body temperature.
- An erysipelas-like form, in which lesions are detected on the skin (sometimes ulcerations appear) that externally resemble erysipelas.
- The armored form is characterized by the presence of multiple nodes, due to which wrinkling and deformation of the mammary gland occurs.
- Paget's cancer affects the nipple and areola. It is characterized by thickening of the nipple, changes in the skin in the form of redness and thickening, and the formation of crusts and scales.
Self-diagnosis
It is worth checking the mammary gland yourself for the presence of nodules or any other changes once a month after menstruation. It is more convenient to carry out home diagnostics while taking a bath or while under the shower. You should tell your doctor about any changes that are discovered as soon as possible.
Procedure for performing breast self-examination:
- Undress from the waist up and stand in front of a mirror.
- Raise your hands up and place them behind your head. Carefully examine the mammary glands. Turn right, left side.
- Feel the mammary glands while standing with your index, middle and ring fingers folded together. Start at the upper outer part of the chest and move clockwise.
- Pinch the nipple with two fingers. Check to see if anything stands out.
- Feel the mammary glands again - now in a lying position.
70% of breast cancer cases are self-diagnosed by patients through breast self-examination.
Examinations before breast reconstruction surgery
Breast reconstruction after removal can be done no earlier than 4 months after completion of radiation therapy and no earlier than 2 months after completion of chemotherapy (targeted treatment). In our institution, we perform such operations under quotas within the framework of the compulsory medical insurance policy (for residents of all regions of the Russian Federation) and for a fee.
Before such an operation, it is necessary to prove that your illness has left you: CT scan of the chest, OSG, ultrasound of the liver. With the results of these examinations, you can contact us to decide on reconstructive surgery.
Diagnosis by an oncologist-mammologist
History taking
Diagnosing breast cancer begins with a conversation. At this stage, it is important for the doctor to evaluate the complaints and find out whether cases of breast cancer have occurred in the family, and if so, how often. This helps to suspect a hereditary form of the disease associated with mutations in the BRCA1, BRCA2, NBS1, CHECK, TP53 genes.
Breast examination
Next, the doctor examines, palpates the mammary glands, checks to see if there are any nodes or lumps in them, or if the lymph nodes in the axillary, supraclavicular and subclavian areas are enlarged.
Instrumental diagnostics
After the examination, the doctor may refer the woman for a mammogram, an X-ray of the breast. Indications for this study include lumps in the mammary gland, changes in the skin, bleeding from the nipple, as well as any other symptoms that may indicate a malignant tumor. Ultrasound examination of the mammary glands is also used. Mammography and ultrasound are complementary methods, each of them has its own advantages:
| Mammography | Ultrasound of the mammary glands |
| Allows you to detect pathological changes in the mammary gland 1.5–2 years before the onset of symptoms. If there is bloody discharge from the nipple, ductography can be performed - X-ray with contrast of the milk ducts. This helps to obtain additional useful information. High sensitivity - accurate diagnosis of up to 90% of cases of breast tumors. Ability to detect microcalcifications up to 0.5 mm. | Safety - there is no effect on the body from x-rays. Well suited for high density breast tissue in young women (up to 35–45 years). Allows you to distinguish breast cysts (cavities with fluid) from solid tumors. Allows you to assess the condition of regional lymph nodes. Well suited for monitoring needle position during biopsy. |
Magnetic resonance imaging is a highly informative method for diagnosing malignant breast tumors. It is used for lobular cancer, when mammography and ultrasound are uninformative, as well as for assessing the size and location of the tumor, which helps determine the tactics of surgical treatment. MRI can be used to screen women who carry abnormal genes associated with an increased risk of breast cancer and have a strong family history.
The final diagnosis is determined by the results of a biopsy. You can obtain breast tumor tissue in different ways:
- Examination of nipple discharge - tumor cells may be found in it.
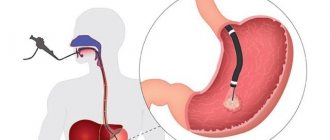
- In a fine-needle biopsy, a needle is inserted into the breast tumor under ultrasound or mammography guidance.
- During a trephine biopsy (CORE biopsy), a special instrument resembling a thick hollow needle is used. It allows you to obtain more breast tumor tissue and examine it in more detail.
- In a needle-gun biopsy, a needle is inserted into the exact location using a special gun.
- A stereotactic vacuum biopsy is almost as accurate as a breast cancer biopsy during surgery, but it can be performed under local anesthesia without the need for general anesthesia. The procedure is carried out using a Bard Magnum pistol and a vacuum apparatus.
- An excisional biopsy is performed during surgery. The entire tumor along with breast tissue is sent for examination.
- Sentinel biopsy is an examination of the sentinel lymph node during surgery. It helps determine whether the tumor has spread to regional lymph nodes and whether they should be removed.
Euroonco doctor S.M. Portnoy talks about the role of biopsy in diagnosing breast cancer:
Cytological and histological examinations are carried out in the laboratory, where the structure of individual cells and tissues is assessed. Molecular genetic studies are currently available: they help to identify mutations that caused malignant degeneration and to select optimal antitumor therapy.
A biopsy can determine whether a tumor is cancerous, as well as determine its type and stage. In addition, examination of the biopsy material provides an answer to the question of whether the tumor is hormone-dependent, which also affects the treatment regimen.
Assessing the extent of cancer spread in the body
Once cancer is diagnosed, it is important to determine its stage and understand how far it has spread. The following studies are used for this:
- Ultrasound and lymph node biopsy.
- Computed tomography and MRI - they help assess the size, location of the breast tumor, and lesions in other organs.
- Metastases in the liver are diagnosed using ultrasound.
- X-rays can help identify lesions in the lungs and bones.
- PET scanning is the modern “gold standard” for diagnosing metastases of malignant tumors.

How often can X-rays, ECGs, mammograms and ultrasounds be done?
The expert explains in what cases radiography can be done several times a year, as well as how safe ECG, mammography and ultrasound are.
Modern diagnostics includes many ways to reliably and quickly obtain an accurate clinical picture of various human diseases in the early stages.
Most of them are associated with the influence of x-rays or exposure to a magnetic field and are not safe for all patients.
Lyudmila Evgenievna Fesenko, an ultrasound doctor at the NEARMEDIC clinic on Maroseyka, told Letidor what risks are fraught with the most common methods of modern functional diagnostics.
Radiography is one of the most common methods of diagnosing diseases; up to 70% of all diagnoses are made on its basis.
This method allows you to identify structural changes and inflammatory processes in the chest, bronchi, nasal sinuses, organs of the gastrointestinal tract, musculoskeletal and vascular systems, and diagnose various tumor diseases, kidney and other pathologies.
How often
When reproducing an x-ray, the patient receives a relatively small dose of radiation, however, x-rays are prescribed according to indications, as well as once a year during clinical examination (in order to exclude pulmonary tuberculosis).
To perform radiography, there are restrictions on the number of sections examined (chest, skeletal studies, etc.) at the same time. This does not apply to patients with severe illness or injury where diagnosis is vital.
When conducting a routine examination, it is recommended to wait 2-3 weeks between repeated examinations.
X-rays are not performed on pregnant women, as X-rays can lead to negative consequences for the development of the fetus.
As for children, since the procedure may not be entirely safe, a referral for such an examination is given in case of emergency, for example, in case of injuries (fall from a height, broken limbs, etc.), including birth injuries, if foreign bodies into the body, asymmetry in the formation of the facial skeleton, before surgery on any organ, if tuberculosis is suspected, etc.
Up to 3 months, x-rays are not recommended at all, and then only in cases of extreme necessity, when it is not possible to make a diagnosis using another method. It is also important to pay attention to the equipment: in modern digital equipment the radiation dose is less than in old film equipment.
An alternative to x-rays is ultrasound and MRI. But in the first case, the picture may be distorted, which will prevent the doctor from making an accurate diagnosis. In the second, it is difficult to persuade a small child to lie still. Therefore, x-rays are the most effective way to identify the problem and prescribe the correct treatment in a timely manner.
Electrocardiography helps diagnose heart disease by recording its electrical impulses, and thus allows you to monitor any deviations in the rhythms of its work.
Unlike other diagnostic methods, ECG does not have any radiation or magnetic fields, therefore it does not harm health and is the safest research method at any age.
How often
An ECG is required during routine examinations, even if there are no symptoms of cardiac dysfunction, as well as before hospitalization and during pregnancy.
Moreover, the number of procedures is not limited: an ECG can be done as many times as necessary to determine the true diagnosis.
Mammography is one of the x-ray research methods that is considered highly effective and informative.
How often
Since this is an x-ray examination, it is prescribed for preventive purposes to women over 40 years old once a year. It is performed in conjunction with ultrasound examination to diagnose diseases of the mammary glands - cancer, mastopathy, cysts and other formations.
https://www.youtube.com/watch?v=3NdQGOUb8r0
Today, ultrasound results are used in various fields of medicine to make or clarify a diagnosis: ultrasound is used to study blood vessels, lungs, bones, the gastrointestinal tract and many other organs and tissues, which was previously considered impossible and uninformative.
How often
A healthy person needs to undergo an ultrasound once a year during routine examinations.
For example, for the purpose of prevention and early detection of cancer or pathologies of the reproductive organs, a woman is recommended to regularly undergo ultrasound of the mammary glands and pelvic organs.
Ultrasounds are performed on children already in the first year - they examine the brain, heart, hip joints, and abdominal organs.
During clinical observation of a person with chronic diseases, including children, the doctor can individually determine the frequency of the study - up to 2-3 times a year, depending on the severity of the disease, periods of remission and exacerbation.
In a normal pregnancy, it is recommended to undergo an ultrasound three times during the entire period or once every trimester.
This is considered optimal in order to monitor its formation and the absence of pathologies or birth defects at certain stages of fetal development.
If a woman has questionable symptoms or if there is a suspicion of fetal malformations, an ultrasound scan is prescribed outside the planned schedule.
Shutterstock/VOSTOCK
Source: https://letidor.ru/zdorove/kak-chasto-mozhno-delat-rentgen-ekg-mammografiyu-i-uzi.htm
Stages of breast cancer
Staging for breast cancer is based on the generally accepted TNM system. The T in this abbreviation indicates the size of the primary tumor:
- Tis is a “cancer in situ” that resides in the cells lining the milk ducts or lobules and does not invade adjacent tissue. This may be lobular, ductal, or Paget's carcinoma.
- T1—tumor diameter in greatest dimension is less than 2 cm.
- T2 - 2–5 cm.
- T3 - more than 5 cm.
- T4 is a tumor that has grown into the chest wall, skin, or inflammatory cancer.
The letter N indicates the presence of metastases in regional lymph nodes. N0 - there are no foci in the lymph nodes. N1, N2 and N3 - damage to different numbers of lymph nodes.
The letter M indicates the presence of distant metastases. One of two numbers can be indicated next to it: M0 - no distant metastases, M1 - distant metastases present.
Depending on the values of T, N and M, there are five main stages of breast cancer (within some of them there are substages):
- Stage 0: cancer in situ.
- Stage I: tumor in the mammary gland up to 2 cm in diameter.
- Stage II: a tumor in the mammary gland with a diameter of up to 5 cm or more, there may be metastases in the axillary lymph nodes on the affected side.
- Stage III: a tumor in the mammary gland up to 5 cm or more, can grow into the chest wall or into the skin, there are foci in the regional lymph nodes.
- Stage IV: The tumor can be of any size, it does not matter whether regional lymph nodes are affected. If distant metastases are detected, stage IV cancer is always diagnosed.
Breast cancer treatment
The treatment regimen for breast cancer should be selected individually for each patient, taking into account factors such as tumor type, stage, and sensitivity of the tumor to hormonal therapy. The general condition of the patient is also taken into account. If the tumor is detected in the early stages and the correct management tactics are chosen, then the chance of completely curing breast cancer is very high.
Surgical method
The surgical method is the dominant one in the treatment of breast cancer. If the tumor is detected early, it is possible to perform an organ-preserving operation—sectoral resection. Performing such an intervention is accompanied by an increased risk of local recurrence, and therefore it is combined with other methods, for example, radiation therapy.
In later stages, breast cancer is treated with a mastectomy—removal of the entire breast along with nearby lymph nodes. The doctor may also decide to remove the second breast if there is a high risk of developing a malignant tumor in it.
A sentinel biopsy, or sentinel lymph node biopsy, may be performed to determine whether cancer cells have spread to the lymph nodes and to determine the extent of surgery . During surgery, a radiopharmaceutical or fluorescent dye is injected into the tumor to help visualize the lymph node that first receives lymph from the breast tissue. It is removed and histological examination is performed. If no tumor cells are found in the sentinel lymph node, you can limit yourself to removing the lesion in the mammary gland. Otherwise, excision of regional lymph nodes is indicated.

Radiation therapy
In order to improve the immediate and long-term results of surgery for breast cancer, radiation therapy is used as an auxiliary method. It can be used in the preoperative period to reduce the degree of malignancy of the breast tumor, damage and regression of micrometastases. However, more often radiation therapy is used after surgery, when it is necessary to destroy cancer cells that may have remained in the body.
Chemotherapy
To treat breast cancer, chemotherapy is used before or after surgery with the aim of complete cure, prolonging life and improving its quality, or to reduce the volume of surgery. Each chemotherapy drug only affects cells in a specific phase of the cell cycle. Therefore, the most effective prescription is polychemotherapy - a combination of several drugs that have different effectiveness and mechanism of action.
Euroonko clinics use the most modern, original European and American chemotherapy drugs for the treatment of breast cancer. We have the opportunity to create a “molecular fingerprint” of the tumor and, based on its analysis, select the most effective and safe combinations of drugs.
Drug therapy: hormonal and targeted drugs
A malignant breast tumor is recognized as hormone-sensitive if more than 10% of the cells in its composition have receptors for estrogen or progesterone. In this case, hormonal therapy is used. The more the tumor has hormonal receptors, the more effective such treatment will be.
This type of therapy includes several methods that stop the production of hormones and block their flow. Today, drugs from the group of non-steroidal antihormones are increasingly used, which affect only the breast tumor and do not affect the mechanisms of hormone formation throughout the body. Therapy with hormonal drugs is prescribed both in the postoperative period to reduce the risk of recurrence, and as an independent treatment for inoperable breast tumors to control their growth.
Targeted therapy is also used to treat breast cancer—drugs that target specific target molecules in tumor cells and have minimal effects on healthy cells in the body. Targeted therapy is used alone or in combination with other treatments.
Fluorography during breastfeeding - recommendations before and after
sh: 1: –format=html: not found
Fluorographic examination is now widely used to identify a number of lung diseases.
Like radiography, this diagnostic method allows you to quickly assess the condition of the respiratory system and determine a preliminary diagnosis. In the future, additional examination is prescribed.
Each of these procedures is absolutely painless, but the body as a whole is exposed to x-rays, which are considered potentially dangerous.
Therefore, many mothers during breastfeeding think about the likely risks of conducting a fluorographic examination.
What is fluorography
Modern medicine has accumulated sufficient practical experience in the use of both fluorography and x-ray diagnostics for examinations of the organs of the bronchopulmonary system. The essence of a fluorographic examination is the passage of x-rays through the human body, reflecting them on a special screen, and only after that it is transferred to film.
But at the same time, pressing questions for nursing mothers remain: is it possible to do fluorography while breastfeeding, is it possible to refuse this examination, and is it necessary to express milk after fluorography.
Modern digital machines scan the lungs using a fan-shaped beam of X-rays, which significantly reduces the radiation dose.
Therefore, if there is a need for fluorography during breastfeeding, you need to clarify what type of device the study will be used on. Radiation doses for different types of fluorography:
Type of examination and radiation dose (mSv)
Film – 0.5 mSv
Digital – 0.05 mSv
Therefore, during lactation, a digital device is preferable to a film one.
Fluorography during breastfeeding, what are the features of the examination
A young mother tries to protect her baby from all possible risks that could harm him, so the question often arises: is it possible to conduct a fluorographic examination if you are breastfeeding your baby.
Many experts argue that fluorography does not affect lactation in any way - the quantity and quality of milk remains unchanged.
Therefore, this type of examination is carried out without restrictions, both fluorography after childbirth and during breastfeeding. At the same time, the health of the mother and baby is practically not threatened even with repeated irradiation procedures.
And yet, no full-fledged studies have been conducted that would definitely confirm that fluorography during lactation is completely harmless.
Therefore, if a young mother is scheduled for fluorography, it is necessary to compare all the factors of potential risk and benefit from this procedure, taking into account the fact that x-rays are, although minimal, irradiation of the body.
When should fluorography be performed during lactation?
But under certain conditions this procedure is mandatory.
A nursing mother must undergo fluorography or a chest x-ray:
- when signs of pulmonary tuberculosis or other chronic respiratory disease or tumors of the chest organs appear;
- upon contact with a person who has a confirmed diagnosis of tuberculosis or whose symptoms are noted;
- if the nursing mother has relatives or friends who have recently been treated for tuberculosis;
- when living in a region where there is an outbreak of tuberculosis;
- if people with whom the young mother has been in contact have a positive Mantoux or Diaskintest test.
Mothers who care about the health of their child need to remember that the epidemiological situation regarding tuberculosis in our country is tense. A woman’s body weakens during pregnancy, so the risk of contracting various viral and bacterial diseases during breastfeeding is higher than that of an ordinary woman.
The possibility of infecting a child with tuberculosis is significantly higher than the risks from radiation exposure during a fluorographic examination
It is important to remember that fluorography during breastfeeding is considered a necessary medical measure to exclude serious diseases that threaten the health of the mother and the newborn or young child. Therefore, the attending physician may insist on taking an image of the respiratory organs if there are serious indications and alarming symptoms.
Young mothers need to know that refusing fluorography if there are strong indications for it may have too high a price in the future - this is worth thinking about.
What recommendations should be followed before and after fluorography?
If there is a need to conduct an examination of the respiratory organs, then the woman should choose for herself the device that is less dangerous during the procedure - digital fluorography or chest radiography.
Many experts confidently say that there should be no restrictions or changes in feeding regimen after fluorography.
But pediatricians still recommend adhering to certain rules in order to protect the child from the possible negative effects of X-ray radiation.
This type of examination can be carried out only if necessary - all preventive examinations are postponed until the end of breastfeeding.
Is it possible to breastfeed after fluorography? This question worries a nursing mother first of all. Pediatricians recommend feeding the baby before visiting the fluorography room.
After the procedure, it is not advisable to breastfeed your baby for two to three hours.
If a situation may arise that the child will want to eat before this time, it is advisable to first express the milk into a bottle. Is it necessary to express milk after fluorography? Experts differ in their opinions on this issue, but if it is better to play it safe and express the milk immediately after the examination.
In the future, the child’s feeding regimen does not change. In the question of whether it is possible to feed the child breast milk after fluorography, some experts recommend delaying feeding the baby for a day or more - this is wrong and often leads to the child refusing to breastfeed or a decrease in the mother’s lactation.
You should not overestimate the potential harm of fluorography for a child and changes in lactation after the procedure - most often these are unfounded fears and breastfeeding after fluorography should be continued as before this diagnostic procedure.
An absolute contraindication to breastfeeding is considered to be only after the mother has confirmed her diagnosis of pulmonary tuberculosis.
Prognosis for breast cancer
If breast cancer is diagnosed in the early stages (0-I), the five-year survival rate approaches 100%. That is, we can say that it is possible to cure almost all patients. Further, depending on the stage, the prognosis for five-year survival worsens:
- At stage II - 93%.
- At stage III - 72%.
- At stage IV - 22%.
The combination of breast cancer treatment methods available to oncologists allows in most cases to achieve remission of the disease or, at a minimum, prolong life while maintaining its quality. The effectiveness of treatment in general directly depends on whether treatment was started in a timely manner.
The maximum effectiveness of antitumor treatment is achieved only if it is carried out in accordance with international protocols and takes into account the individual characteristics of each patient. This is exactly how Euroonco oncologists prescribe treatment.
| More information about breast cancer treatment at Euroonco: | |
| Surgeons-oncologists-mammologists | from 5100 rub. |
| Removal of a breast tumor | from 92,000 rub. |
| Emergency oncology care | from 11000 rub. |
Book a consultation 24 hours a day
+7+7+78
Where to undergo examinations after breast surgery
On the “ Where to be examined ” page, the coordinates of specialists who have proven themselves to be conscientious in St. Petersburg will open.
Formally, examinations should be carried out by oncologists in local clinics. But there are problems here:
- The amount (compensation from insurance companies for examinations) does not cover their cost. Therefore, clinic doctors can only prescribe what is regulated by them for patients. For example, if money is allocated to provide ultrasound, and the patient needs to have a computed tomography or magnetic resonance imaging, or PET scan (as more informative diagnostic methods), then only ultrasound can be provided.
- If an oncologist is prescribed, for example, 3 computed tomography scans for all his patients for six months, then he will not prescribe this examination for the fourth patient, even if he himself knows that she “really needs it.”
- If the examination did not reveal any pathology (metastases were not found), then this is interpreted as an “off-label prescription.” For this, the doctor receives reprimand, and the insurance company may refuse to pay the clinic for the doctor’s labor and reimbursement for examinations performed “not according to indications.”
- Some examinations are not standard in countries with low levels of healthcare funding, so, for example, patients are often not even told about OSG, CT or PET.
- Patient complaints lead to the dismissal of their doctor, since the medical administration. institutions interprets informing patients about the lack of anything for their treatment and examination - only as an action provoked by doctors against the administration. Therefore, doctors prefer not to say that something is missing, but to explain it by saying that “You don’t need it” or “we have something to replace it with.”
Therefore (most often) examinations are prescribed only when early signs of the return of the disease have already been missed, and signs of dysfunction of the affected organs appear.
Another nuance is whether you undergo examinations by experienced specialists or not, on modern equipment or outdated ones.
You should know that today in the country there is no legal mechanism for rewarding well-performing doctors. The work of the doctor who sees you at the clinic under the compulsory medical insurance policy is valued by the state at 50 rubles (about 1 USD): that is how much the state pays him for the fact of your appointment (your consultation). The quality of work is not assessed. The doctor has nowhere to go; the rules of work are the same everywhere. To make money, he takes more consultations, incurring losses in quality. Be prepared that for a high-quality modern examination from good specialists you will have to bear the costs, or somehow stand out from the general background of other patients (in order to draw his attention to your problems and become interested in doing more for you than is regulated). Or your observation and examination - like in a lottery, will largely depend on chance.
If the information on our website was useful to you, please leave your reviews about it and recommendations on the Internet for other patients.