Today, ultrasound diagnostics is rightfully considered one of the safest and most informative. It is applicable in various fields of medicine, and is also used to determine abnormalities in the vascular system. If there is a need to study blood vessels, TCDG is used, which stands for transcranial Dopplerography of cerebral vessels.
Transcranial Dopplerography of cerebral vessels: what is it?
TCD is based on ultrasonic waves and the Doppler effect. Ultrasound waves are reflected from moving red blood cells and vessel walls, and with the help of a special sensor and software, the pulses are converted into an image that is displayed on a computer screen.
TCD of cerebral vessels will determine the condition of the main arteries, which are responsible for supplying the brain with oxygen, as well as other large arteries and vessels. Thanks to this, it will be possible to assess the condition of the vessels and determine the speed and intensity of blood flow in them.
When is the study carried out?

A diagnostic procedure is performed to confirm or monitor the following diseases:
- Vegetovascular dystonia;
- Osteochondrosis of the cervical spine;
- Tremor and feeling of numbness in the limbs;
- Acute disorders of cerebral blood flow;
- The appearance of tinnitus;
- Spinal column injuries;
- Migraine and frequent headaches;
- Heart attack and coronary heart disease;
- Frequent dizziness and fainting;
- Decreased visual acuity;
- Head injuries;
- Obesity and diabetes;
- Violations of the functionality of the vestibular apparatus;
- Genetic predisposition to vascular pathologies.
TCD is a safe and accurate diagnostic method that is widely used to study cerebral vessels.
The procedure successfully competes with other modern techniques due to its ease of implementation and accessibility. Transcranial Dopplerography has no contraindications and does not cause complications. Therefore, the method is widely used to monitor vascular pathologies of the brain. During the study, it is necessary to strictly follow the doctor’s instructions, which will significantly increase the information content of the method. Which method is safer? The main pros and cons of ultrasound, MRI and CT
Indications for transcranial Doppler ultrasound
There are many reasons why you may need to undergo Doppler ultrasound. Transcranial Dopplerography of cerebral vessels
may show a large number of deviations from the norm.
Vascular malformation
It is a congenital disease that affects the development of the vascular system. Manifests itself in the form of plexuses of abnormal vessels of various sizes. It is dangerous because it can cause subarachnoid hemorrhage of a non-traumatic nature. Among other things, steal syndrome may develop, and malformations may begin to compress the brain tissue.
Cerebral circulatory disorders
TCD is used quite often to examine cerebral vessels. It may be necessary to identify the cause of problems with cerebral circulation. They may consist of the formation of blood clots, loops and kinks in blood vessels. Often the cause is: the formation of narrowings, aneurysms or embolism.
Atherosclerosis of the arteries of the neck and head
It consists of damage to areas of blood vessels by atherosclerotic plaques, which either significantly narrow the lumen of the vessel or clog it completely. In advanced cases, treatment is performed surgically. TCD is used to examine vessels because it allows one to determine not only the presence of plaques, but also their size and location.
Encephalopathy
Occurs in chronic cerebral vascular diseases that slowly progress. This disease combines cognitive impairment, disruptions in the emotional and motor spheres.
Research methodology

It is important not only to understand what it is - TCD of cerebral vessels, but also to know how such a procedure is carried out. During this procedure, the patient will need to lie on his back, at which time the doctor will apply a special gel to the area being examined, after which he will apply a sensor and move it along the course of the arteries. You may need to breathe more frequently and also turn your head in certain ways. Unpleasant sensations during TCD to examine the cerebral vessels are excluded; the patient only feels the pressure of the sensor.
What vessels can be studied using TCD?
The position of the acoustic window will determine the list of blood vessels that can be examined. There are only three windows:
- temporal;
- orbital;
- suboccipital.
Examination of the brain using the TCD method using a temporal window will allow you to examine the internal carotid artery, middle, anterior and posterior cerebral arteries. Involves examination through the temporal region.
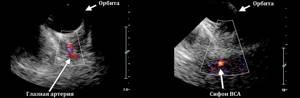
Orbital window - scanning the arteries through the orbits of the eyeballs. Allows you to assess the condition of the ophthalmic artery and the internal carotid siphon.
The suboccipital window involves ultrasound examination through the junction of the occiput with the spine. The basilar artery is examined, as well as the intracranial segments of the vertebral blood vessels.
Neurosonography and TCD
If you do not know what kind of examination TCD and neurosonography
, then you should understand that it applies to infants. In fact, this is an ultrasound of the child’s brain, which is completely safe and allows you to see the early manifestations of various abnormalities.
How is the procedure performed?

TCD is an absolutely painless examination, during which the patient does not experience any discomfort or discomfort.
The study takes no more than 15-20 minutes.
The accuracy of the results obtained is determined by the placement of the sensor and the position in which the patient is located. More often, TCD is performed with the patient sitting or lying on his back, with a small cushion placed under his head. But if the doctor doubts the reliability of the information received, the patient will need to lie on his stomach or side.
During transcranial Doppler ultrasound, the patient should not talk, move or change head position. To determine blood flow, the doctor places a sensor with slight pressure in the area of the back of the head, temples, neck, and forehead. To assess the functional activity of blood vessels, you may need to hold your breath for a while or take several intense breaths.
What does transcranial Doppler sonography show?
After you have learned what TCD is, it is worth familiarizing yourself with the data that will become known as a result of the procedure. The following will be taken into account:
- vein or artery wall thickness, diameter;
- minimum and maximum blood flow speed, its nature;
- resistive and ripple indices.
Each of these indicators may indicate the presence or absence of disease.
The speed of blood flow through the arteries
A TCD examination may show an abnormality, which is a deterioration in blood flow. The cause may be the presence of blood clots or plaques, as well as other problems that can be identified through duplex testing.
Venous drainage from the cranial cavity
There can be many reasons for this phenomenon; they may include severe traumatic brain injuries, the occurrence of tumors that compress blood vessels and/or brain tissue. Often, outflow occurs against the background of a stroke and its consequences, with a decrease or underdevelopment of the network of blood vessels.
Degrees of development of the collateral network of brain vessels
TCD examination can reveal underdevelopment of the blood vessel network. It often causes problems with blood supply to the brain. All detected violations are recorded in the conclusion.
Transcranial Doppler (lecture at Diagnostic)
The article is under development.
Transcranial Doppler sonography is useful for diagnosing embolism, stenosis, vasospasm after subarachnoid hemorrhage, vascular deformation, etc.
In order for the ultrasound beam to pass through the skull bone, a 1-2.5 MHz sector sensor is used. The wall and lumen of the vessels are not visible in B-mode; a “colored” cast and flow velocity are examined.
For temporal and orbital access, the patient is in the supine position; access through the foramen magnum from the back of the head.

Orbital access through the upper eyelid with the patient's eyes closed; the ophthalmic artery and a cross-section of the ICA siphon can be seen.
Access through the temple anteriorly, above and posteriorly from the auricle: you can see the MCA, ACA, PCA, PSA, PCA, transverse section, SMV, veins of Rosenthal and Galen, straight sinus.
Access through the foramen magnum: you can see the PA and OA, P1 and P2 segments of the PCA, cerebellar arteries; straight sinus, venous plexuses of the base of the skull.
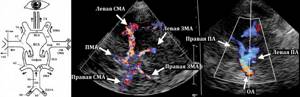
TKDS begins with a general examination of the brain structures in B-mode, assessing the presence of pathological formations in them. The midbrain is a “butterfly” of medium echogenicity. The “butterfly” is surrounded by a pulsating structure—the PCA.
The temporal horns of the lateral ventricle are defined in the temporal lobe as oblong-shaped hypoechoic structures containing a hyperechoic choroid plexus.
The base of the skull has a high echo density. The hyperechoic lesser wings of the petrosal and sphenoid bones, which form the border of the middle cranial fossa, are its main landmarks.
Parallel to them, in the hypoechoic Sylvian fissure, there is a pulsating structure corresponding to the trunk (segment M1) of the middle cerebral artery (MCA).
When the sensor is slightly tilted cranially, the ovoid-shaped thalamus is visualized. The pineal gland has increased echo density.
The third ventricle and interhemispheric fissure are visualized as midlinear structures of increased echo density. In the area of the interhemispheric fissure, pulsation of the anterior cerebral artery (ACA) is detected, on the sides of the interhemispheric fissure there are somewhat asymmetrical, elongated horns of the lateral ventricles.
The anatomical landmark when scanning the MCA, ICA siphon, ACA, SMV is the hyperechoic pyramid of the temporal bone; segment A1 of the ACA in the projection of the interhemispheric fissure; PCA, vein of Rosenthal, diameter of the OA near the cerebral peduncles; vein of Galen, straight sinus and sinus drainage zones in the area of the thalamus and third ventricle.

All arteries supplying the brain have low peripheral resistance: high velocity in diastole and low IR. In paired arteries the difference in flow velocity is up to 30%, IR is up to 10%.
Quantitative indicators of blood flow in healthy individuals are variable and depend on blood pressure, time of day, emotional background, time since the last cigarette was smoked, and the phase of the menstrual cycle.
About 55% of the total blood volume enters the MCA, 20% into the ACA and 25% into the PCA. In adults, the normal linear velocity of blood flow in the MCA is 75±15 cm/sec, the ACA is 49±11 cm/sec, and the PCA is 38±11 cm/sec.
SMA red, spectrum above baseline as flow is directed towards sensor, TAMX 122 cm/s. The anterior cerebral artery of segment A1 is blue, the spectrum is below the baseline because the flow from the sensor is directed towards the midline of the brain.

The most commonly used is the time average maximum speed (TAMX), also called average speed. Peak systolic velocity (VS) and end-diastolic velocity (VD) can also be measured.
With local narrowing of the artery or spasm, TAMX increases in the 5-10 mm segment by 30 cm/s compared to the opposite side.
High TAMX with stenosis, vasospasm, hyperdynamic flow, low hematocrit; low TAMX for arterial hypotension, brain stem death.
Table. Time-averaged maximum velocity (TAMX) in basal vessels (Aaslid, 1982)

Two indicators reflecting vascular peripheral resistance can be calculated. The normal PI ripple index is 0.7-1.1. The resistive index RI after the neonatal period is 0.5 ± 15% (0.43-0.58).
These two indices always move in the same direction. When flow resistance is low during diastole, flow velocity is higher and RI and PI are reduced.
For example, downstream of severe stenosis due to ischemia, PCO2 increases and vasodilation occurs.
Intracranial hypertension due to a diffuse increase in resistance leads to increased indices.
Velocity in intracranial arteries increases with high volume flow or stenosis. Stenosis less than 50% does not lead to significant hemodynamic disturbances. The condition of the extracranial vessels affects the result.
In the ICA siphon, due to physiological bending, it is difficult to install the sensor at the correct angle; Indirect signs of stenosis in this zone are considered to be similar spectrum changes in the MCA and ACA.
Aneurysms occur in the ACA, PCA, supracuneiform part of the ICA, MCA and OA; a round colored spot is adjacent to the main vessel; Blind areas with thrombi make it difficult to estimate size.
With TCD, venous structures of the brain are visible: superior sagittal sinus 0-54%. transverse sinus 20-73%, drain sinus 17-53%. When the blood flow velocity is less than 4 cm/sec, the vessel is not detected on TCD.
The deep venous system is examined through the temple on an axial section through the diencephalon, where the dorsal parts of the thalamus and the occipital lobes of the telencephalon are visible. Parallel to the middle cerebral artery is the deep middle cerebral vein.
The straight sinus is a blue-colored punctate structure located in the dorsal part of the midline; in some cases it is possible to visualize its flow into the sinus drainage. The sinus drainage is determined caudal to the straight sinus and projects somewhat asymmetrically onto the contralateral occipital bone. Anterior to the direct sinus, in the middorsal part of the diencephalon, a blue-colored tubular structure is identified - the great cerebral vein, or vein of Galen, into which the internal and basal veins of the brain flow.
The straight sinus is visualized through the back of the head; It is also possible to obtain images of the superior and inferior sagittal sinuses. Normally, the spectrum of the Doppler frequency shift in the veins of the brain has a weak phasic pattern.
Table 2.10.
Indicators of blood flow velocity in the deep veins of the brain and sinuses are normal
Vasospasm
Flow rates are inversely proportional to the diameter of the vessel and directly proportional to the degree of vessel narrowing or stenosis until a critical stenosis is reached at which flow rates actually decrease. In general, the narrower the diameter of the vessel and the greater the severity of vasospasm, the higher the flow rate.
Vasospasm after subarachnoid hemorrhage is usually absent in the first 72 hours. Vasoconstriction usually occurs on day 3, peaks between days 6 and 12, and resolves 15 to 20 days after the onset of hemorrhage.
Subarachnoid hemorrhage due to a ruptured aneurysm can lead to cerebral vasospasm, which is associated with a 15% to 20% risk of stroke or death. Radiologically detectable vasospasm is estimated to occur in 50–70% of patients after aneurysm rupture, with approximately half of those affected developing clinical signs and symptoms, usually within 3–14 days after the onset of hemorrhage.
Parameters used to detect and measure vasospasm on transcranial Doppler include PSV, MFV, and various indices (eg, RI).
An increase in flow rate alone is not a sufficient basis for a confident diagnosis of vasospasm; Physiological conditions such as hyperemia and autoregulation, and induced conditions such as hypertension and hypervolemia can also result in increased or decreased flow rates.
To correct for and differentiate between these dynamic states, Lindegaard proposed using a ratio derived from simultaneous measurements of MFV in the MCA and the distal ipsilateral extracranial ICA (MFVSMA/MFVBCAec).
The Lindengaard index allows you to distinguish between hyperdynamic blood flow and vasospasm in the MCA: MFVСМА/MFVВСАneck. The modified Lindengaard index allows you to distinguish vasospasm in OA: MFVОА/MFV (middle VA of the neck). The Sloan coefficient shows vasospasm of the ACA: MFVPCA/MFVBCAneck.
Stenosis It has been shown that transcranial Doppler sonography can reliably exclude the presence of intracranial vascular stenosis. However, although transcranial Doppler findings (eg, increased flow velocity, turbulence) may indicate the presence of stenosis, these findings must be confirmed by conventional angiography or CT angiography before a diagnosis can be made.
CT angiography of the circle of Willis shows severe short segment stenosis of the M1 segment of the right MCA (arrow). Although severe vasospasm may have the same appearance, atherosclerosis is believed to be the cause of the stenosis because vasospasm usually affects a longer segment of the vessel and because Despite clinical signs and symptoms of stroke, no subarachnoid hemorrhage was detected on unapproved CT.
ICA occlusion
Ultrasound findings of extracranial ICA occlusion include echogenic material filling the vessel on grayscale imaging and absence of flow on color Doppler flow imaging and Doppler spectra. In addition, the shape of the ipsilateral common carotid artery changes from low to high resistance.
When occlusion is present, a collateral pathway can form in which the ipsilateral external carotid artery supplies the OA, which in turn can supply the brain via the MCA. When this pathway is present, the waveform in the external carotid artery becomes “internalized” (converted from a high-resistance flow pattern to a low-resistance pattern) and the flow within the OA is reversed. Flow reversal in the OA can be demonstrated on transcranial Doppler using a transorbital approach.
ICA stenosis with collateral circulation. (a) Power Doppler flow US image shows echogenic material filling the right ICA (arrows). The flow was not identified using either power Doppler or spectral Doppler techniques. These findings indicate ICA occlusion. (b) US color Doppler image and spectral Doppler waveform show low-impedance inward flow in the right external carotid artery. (c) Transcranial Doppler image obtained using the transorbital approach shows reversal of blood flow in the right OA, indicating collateral flow from the external carotid artery to the MCA through the right OA. (d) US transcranial Doppler image obtained in the left OA for comparison shows normal flow.
Tags: head Doppler lectures ultrasound neck