The soft tissues of our body include the skin, subcutaneous fat layer, lymph nodes, muscles and joints. They make up about half of the body's total mass. The ultrasound method allows you to examine soft tissues in detail, determine their structural changes and diagnose pathology at an early stage of its development.
- What is soft tissue ultrasound?
- Types and features
- Indications and contraindications for ultrasound of soft tissues
- How is soft tissue ultrasound performed?
- What parameters are noted in the ultrasound protocol?
- What can be revealed
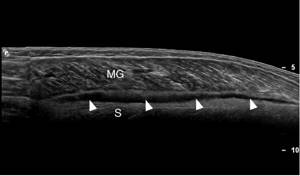
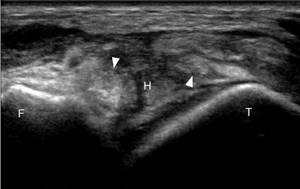
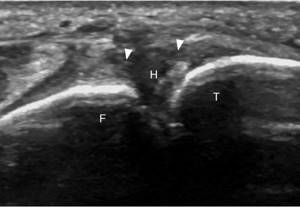
Rupture of the medial head of the gastrocnemius muscle
A tear of the medial head of the gastrocnemius muscle, called “tennis leg,” most often affects middle-aged athletes who report sharp pain in the middle of the lower leg while actively plantar flexing the ankle and extending the knee.
When evaluating symptoms suspicious for rupture, the physician should consider the alternative diagnosis of deep vein thrombosis, which may also be associated with the symptoms.
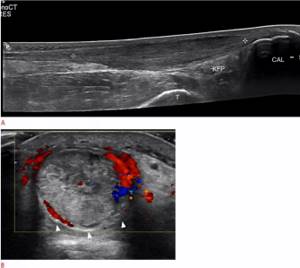
The medial head of the gastrocnemius muscle is best assessed in the longitudinal plane. Ultrasonic characteristics of the rupture include disruption of the normal alternating linear hyperechoic and hypoechoic appearance at the distal myotendin junction, where hypoechoic hemorrhage replaces the normal cone-shaped appearance of the distal aspect (Fig. 10).
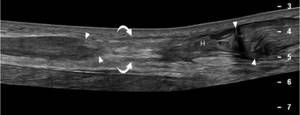
Large tears are characterized by retraction and heterogeneous fluid extending proximally between the muscle bellies of the medial head of the gastrocnemius muscle and the plantar muscle.
Figure 10 : 30-year-old woman with a medial gastrocnemius head rupture (tennis leg). Ultrasonography of the long axis of the tibia to the distal medial head of the gastrocnemius muscle (MG) demonstrates an irregular and hypoechoic distal myotendin junction (arrowheads) with a small hypoechoic hematoma (curved arrows) between the MG and soleus muscle (S).
Compare with normal muscle appearance (arrows).
Who interprets the results and how to obtain them?
The radiologist, a doctor specially trained to monitor and interpret x-ray studies, will analyze the images and send a signed report to your primary care physician or other health care provider who requested the analysis. Typically, the referring doctor or health care provider will share the results with you. In some cases, the radiologist may discuss the results with you at the end of your examination.
Follow-up inspections may be required. Your doctor will explain the exact reason for requesting another test. Sometimes follow-up testing is done because the potential abnormality needs further evaluation with additional views or special imaging techniques. In addition, follow-up testing may be required so that any change in the known abnormality can be monitored over time. Follow-up examinations are sometimes the best way to see whether treatment is working or whether the result is stable or changes over time.
You can sign up for a consultation and find out more from the administrator by calling +7 (495) 356-30-03.
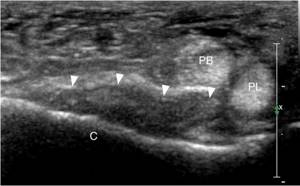
Sole tear
Patients with a plantar tendon rupture describe a sudden onset of pain in the gastrocnemius muscle that feels as if they have been punched or directly impacted, similar to patients who have sustained an injury to the medial head of the gastrocnemius muscle.
The plantaris muscle originates along the posterior superior aspect of the lateral femoral condyle, with the muscles extending downward and medially along the back of the knee. The long, thin plantar tendon, located between the plantar and medial heads of the gastrocnemius muscle, ends either on the calcaneus adjacent to the posterior medial aspect of the Achilles tendon or on the Achilles tendon itself.
On ultrasound, a plantar joint tear is diagnosed by the absence of a normal plantar joint tendon with heterogeneously hypoechoic fluid representing a hematoma at its presumed location between the plantar and medial head of the gastrocnemius muscle (Figure 11).
How is soft tissue ultrasound performed?
Patients do not need to prepare before the procedure. The examination can take place either sitting or lying down. The patient's position depends on the area being examined. In the referral for ultrasound, the attending physician indicates the probable location of the pathology and the primary diagnosis.
Before starting the procedure, the patient must remove clothing from the area being examined. Next, the sonologist applies the gel to the ultrasound probe or the patient’s skin. The gel ensures continuous contact of the sensor with the skin. If air bubbles get in the way of the ultrasonic waves, the image will be distorted and the results obtained will be inaccurate. To prevent this from happening, use a gel layer. The gel is based on glycerin, which does not cause allergic reactions. After the procedure, simply remove it with a napkin.
An ultrasound machine sends and receives ultrasound waves, then converts the received data into an image on a monitor. The ultrasound specialist uses it to determine the pathology of soft tissues. The data obtained is recorded in a research protocol, which is given to the patient at the end of the procedure.
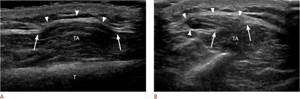
Achilles tendon injury
Achilles tendon injury typically affects athletes in the third to sixth decades of life and is the result of sudden or repeated resistance dorsiflexion.
Anatomically, the tendon receives bundles from the medial and lateral heads of the gastrocnemius muscles, as well as from the sole. Although there is variability as the tendon progresses distally, rotation of the tendon fibers occurs approximately 90° so that fibers from the plantaris muscle that are deep proximally become medial when inserted into the calcaneus.
Unlike other tendons, the Achilles tendon does not have a tendinous sheath. Instead, the Achilles tendon is surrounded by a single layer of cells called the paratenon.
On ultrasound examination, a normal paratenon is defined as a thin, slightly echogenic line encapsulating the tendon. Inflammation of the highly vascular paratenon leads to pain in the back of the ankle and is called paratenonitis.
The inflamed paratenon swells with fibroblasts and inflammatory exudate, resulting in thickening and a hypoechoic appearance on ultrasound. (Fig. 12)
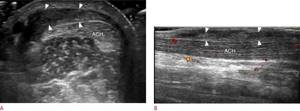
Injury to the Achilles tendon can occur at the myotendin junction, an area approximately 2-6 cm proximal to the insertion, commonly called the "critical zone" or less commonly at the calcaneus.
Typically the tendon is hyperechoic, fibrillary, and has uniform thickness along its long axis. Tendinosis may present as fusiform thickening and hypoechogenicity of the tendon with possible hyperemia due to neovascularization, which correlates with the patient's symptoms (Figure 13).
Anechoic clefts are partial ruptures; thickening of the tendon to more than 10 mm with internal heterogeneity indicates partial rupture in addition to tendinosis. Hyperemia on color Doppler and distension of the retrocalcaneal bursa (greater than 2.5 mm) may further confirm this latter diagnosis.
In cases of complete, full-thickness Achilles tendon rupture, there is retraction of the proximal tendon fibers and a positive Thompson test, where compression of the tibia does not result in normal plantar flexion of the foot.
On ultrasound, the retracted tendon fibers are wavy and irregular with heterogeneously hypoechoic intervening fluid. It is important to document both the quality of the stumps and the residual gap between the tendon stumps during dorsiflexion as this helps guide clinical decisions regarding surgical and nonsurgical treatment (Figure 14). Full thickness tears are present as tendon tears and retraction during dynamic assessment with passive plantar flexion and dorsiflexion.
The use of dynamic imaging that demonstrates a tendon rupture is an important component of ultrasonography to achieve high accuracy in diagnosing a full-thickness rupture.
What is soft tissue ultrasound?
Ultrasound (echography, or sonography) is a non-invasive method for diagnosing organs and soft tissues of the body using ultrasonic waves. Ultrasound travels through the body in the form of alternating waves that are reflected differently from structures with different densities. The device picks up these changes and converts them into a picture.
For ultrasound of soft tissues, as a rule, linear sensors with a frequency of 5-10 MHz are used. The depth of propagation of waves of this frequency does not exceed 10 cm, but the resulting image has a high resolution with an accuracy of up to a millimeter. Sensors with this frequency cannot detect pathology that has formed deeper than 10 cm. In this case, lower frequencies (2-3.5 MHz) are used for diagnosis. The same frequencies are used for ultrasound of the abdominal organs.
Sonography allows you to visualize the internal structure of soft tissues. The examination procedure takes 10-20 minutes, does not require preparation and is safe for the body. Ultrasound can quickly assess injuries caused by injuries, which is why this method is indispensable in emergency medicine. An X-ray image gives the surgeon an idea only of the condition of the damaged bone, and an ultrasound image shows ruptures and hematomas of soft tissues.
Ultrasound is harmless to the body, so the procedure can be performed at any age. Ultrasound of soft tissues is a fast, informative, accurate and affordable diagnostic method that you can find in any clinic in Moscow.
Peroneal tendinopathy
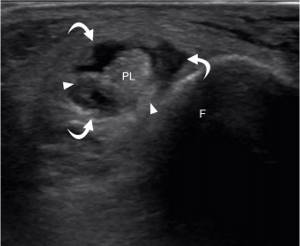
A common cause of posterolateral pain in the ankle joint is the peroneal tendons, which are susceptible to injury. While the peroneus longus muscle (FMM), arising proximally from the fibula and tibia, has its myotendin junction long before it reaches the ankle, the peroneus minor muscle (FMM), arising from the distal fibula, tapers distally to the lateral ankle, where the tendons pass posteriorly in the retromalleolar groove. The MMM is usually in contact with the fibula between the bone and the DMM, which likely explains its susceptibility to injury at this location.
On ultrasound examination, perineal tendinosis appears as hypoechogenicity with possible tendon enlargement. Anechoic clefts indicate a superimposed rupture. An anechoic cleft that extends into the surface of the tendon, usually the MMM, is called a longitudinal tear fracture (Fig. 15).
A full thickness rupture is a tendon rupture with retraction.
What does MRI of muscles and superficial structures show?
MRI makes it possible to detect changes in muscles and superficial structures caused by diseases, injuries and other causes, including developmental abnormalities, in the early stages, and to take adequate therapeutic measures in a timely manner.
At the same time, MRI allows you to detail the smallest structures such as individual muscle bundles, tendon fibers, etc.
Soft tissue MRI helps:
- identify the presence and location of the source of inflammation or infection;
- determine the presence of post-traumatic changes;
- identify neoplasms in soft tissues, etc.
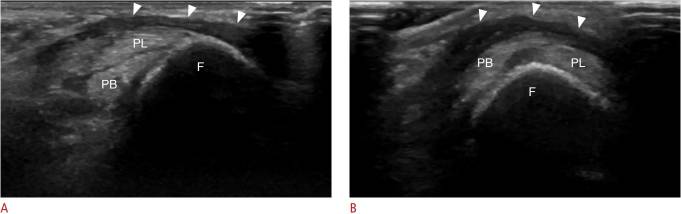
Subluxation and dislocation of the peroneal muscles
Abnormal peroneal tendon movement can result in popping, pain, and tendon damage and is best assessed with ultrasound during dynamic imaging with ankle flexion and inversion.
Tendon subluxation and dislocation result from damage to the superior perineal retina, which normally holds the tendons along the posterior fibula in the retromalleolar groove.
When damaged or ruptured, the retina may be hypoechoic or discontinuous, with or without an avulsed fragment. During stress maneuvers with dorsiflexion and eversion, one or both peroneal tendons may be partially displaced anteriorly and laterally from their normal position (subluxation) or completely displaced (dislocation) and return during rest. (Fig. 16)
How is the procedure performed?

For some musculoskeletal ultrasound examinations, the patient may sit on an examination table or swivel chair. For other ultrasound examinations, the patient is positioned face up or face down on a couch. The radiologist or sonographer may ask you to move or guide the limb being examined to evaluate the anatomy and function of the joint, muscle, ligament, or tendon.
Most ultrasounds of infants and children are performed with the child lying on his or her back on a couch, but a different position may be required.
Once you are on the examination table, a radiologist (a doctor specially trained to observe and interpret x-rays) or sonographer will apply a warm, water-based gel to the area of the body being examined. The gel will help the sensor make safe contact with your body and eliminate air pockets between the sensor and your skin that could block sound waves from entering your body. The transducer is placed on the housing and moved back and forth across the area of interest until the desired images are captured.
As a rule, there is no discomfort from pressure when pressing the sensor on the area being examined. However, if the scan is performed in an area that is too sensitive, you may feel pressure or slight pain from the transducer.
Once the image is acquired, clear ultrasound gel will be wiped off your skin. Any parts that are not washed dry quickly. Ultrasonic gel does not typically stain or discolor clothing.
Anterior talofibular ligament rupture
One of the most biomechanically important ligaments of the ankle, the anterior talofibular ligament (ATFL) is also the most common injury and results from abnormal inversion stress.
To identify the ligament, either palpate or locate the extreme distal end of the fibula using ultrasound in the transverse plane. Then move the sensor forward slightly until the fibula and talus are in view. An obliquely oriented PTF may be slightly hypoechoic with anisotropy, but changing the transducer angle with a heel-toe maneuver should reveal a normal echogenic fibrillary pattern.
Injuries to the PTJ result in symptoms similar to other ligament injuries. In acute partial rupture, the ligament is hypoechoic with some intact fibers remaining. In an acute full-thickness tear, the fibers are intermittent or absent and are replaced by a heterogeneous hematoma (Fig. 17). Avulsion tears are identified as echogenic lesions adjacent to areas of ligamentous attachment. Dynamic imaging can help distinguish between partial and full thickness tears.
In a chronic tear, the ligament may be absent, thin, or thickened, but the patient should have no associated symptoms with the pressure of the transducer. If injury to the lateral ankle ligament is suspected, the calcaneofibular ligament, which appears as a hypoechoic and thickened ligament adjacent to the body of the calcaneus, should also be assessed (Figure 18).
Sign up for ultrasound diagnostics
In the medical center, ultrasound examinations are performed using expert-class equipment.
The appointment is conducted by doctors:
– GONTAREV ALEXANDER GENNADIEVICH,
– ZHEVED ELENA SERGEEVNA,
– MAKOVEEVA IRINA SHAUKATOVNA
professional diagnosticians with extensive practical experience.
Ultrasound examinations in the clinic are carried out by appointment.
Phone number for registration.
Address: Sevastopol, Heroes of Stalingrad Avenue, 63
(stop b. Omega)
Opening hours: Mon. - Fri: 07:30 - 17:00, Sat. — Sun: 08:00 — 16:00
The patient should check with the administrators about the need for additional preparation for diagnosis.
The cost of ultrasound of superficial organs is 900 rubles.
Ankle sprain
During an ankle sprain, the first syndesmotic ligament of the ankle to be injured is the anterior inferior tibial ligament (ITI).
Identification: first we orient the sensor over the anterior talofibular ligament, then rotate the medial side of the sensor so that it is inclined and the fibrillary ligament is in the field of view. The resulting imaging plane should be similar to that of the calcaneofibular ligament, but on the tibial side of the fibula.
Ligament tears will appear as hypoechoic thickening or interruption of continuity (Figure 19).
However, if the PNJ has been injured, then injury to the interosseous membrane, commonly referred to as an “ankle sprain,” should be ruled out as it may result in delayed healing and recovery, instability, and accelerated degenerative changes.
The interosseous membrane is identified as a thin echogenic linear structure between the tibia and fibula and may be discontinuous, thickened, and hypoechoic when injured. Dynamic imaging can be a useful tool to assess integrity, assessed by measuring the free space in the tibia at 1 cm from the joint line.
Typically there should be a minimal difference in tibial headspace measurements between internal and external rotation at the ankle (typically less than 2 mm difference, but up to 5 mm). A significant expansion of free space during external rotation indicates damage to the interosseous membrane.
What can be revealed by ultrasound of soft tissues?
Using ultrasound waves, benign tumors can be detected - lipoma and atheroma (sebaceous gland cyst), as well as malignant neoplasms - sarcoma and melanoma. On an ultrasound image they appear as hypoechoic formations (areas of low density), they can have a homogeneous or heterogeneous structure. This depends on the type of tumor. To clarify the diagnosis, the patient is prescribed additional diagnostics.
Ultrasound allows you to study a hematoma - an accumulation of blood or fluid that forms due to rupture of blood vessels during injury. Small hematomas are not dangerous to the body; over time they resolve on their own. Large hematomas are removed surgically. Fluid suppurates in them, which is accompanied by pain and increased body temperature.
Ultrasound of the neck and face is performed to study tumors and inflammatory processes. A plastic surgeon can use ultrasound to monitor inflammatory and adhesive processes after tightening. Ultrasound of the neck is performed in newborns with pathology of the lymph nodes and torticollis - a disorder of the musculoskeletal system.
Ultrasound of joints can detect dislocations, ligament tears, nerve damage and inflammatory processes. In the area of the joints, you can find a hygroma (joint hernia) - a benign cystic formation. It is filled with serous fluid mixed with mucus or fibrin. On ultrasound it appears as an anechoic formation.
Ultrasound of the soft tissues of the leg can detect various compactions, a hernia of the hip and popliteal joint (Baker's cyst), fractures of the thin bones of the foot and a heel spur. A heel spur is a thin bony growth on the heel that is shaped like a spike or wedge. This pathology is accompanied by pain when walking and requires treatment.
Ultrasound diagnostics of the soft tissues of the abdomen makes it possible to study tumors and abdominal hernia - a pathology in which internal organs extend beyond their position. This pathology can be congenital or acquired. To study it, you may need not only an examination of the soft tissues of the abdomen, but also an ultrasound of the entire abdominal cavity. Check this point with your doctor, because certain preparation is required before abdominal sonography.
Muscle hernia
Muscle hernias often present a diagnostic dilemma. A muscle hernia occurs when a normal muscle protrudes from its normal anatomical compartment through a defect in the overlying fascia. 89% of muscle hernias occur in the lower extremities, most often involving the tibialis anterior muscle, but also often involving the fibular muscles. Pain associated with this object may be due to transient muscle strangulation or superficial nerve entrapment; however, some have described a correlation with chronic compartment loading syndrome, which may serve as an alternative etiology of pain.
DO YOU CARE CORRECTLY FOR YOUR ULTRASOUND DEVICE?
Download your care guide now
Download PDF
During ultrasound evaluation, several technical considerations may improve diagnostic accuracy. The mass should be manually palpated and marked by hand.
Normal fascia should appear as a thin echogenic line directly overlying the muscle. A muscle herniation is diagnosed when imaging demonstrates a defect in the echogenic fascia with part of the underlying muscle protruding through and above the fascia, often taking on a mushroom shape (Figure 20). Muscle herniation may be somewhat less echogenic than adjacent normal muscle and may be secondary to anisotropy or atrophy. Blood vessels are sometimes noted to cross the fascia at the site of the defect and have been suggested as a potential cause of focal fascial laxity.
Indications and contraindications for ultrasound of soft tissues
Reasons for performing an ultrasound of soft tissues may include:
- enlarged lymph nodes,
- pain of various types,
- formation of compactions in soft tissues,
- muscle hernias,
- suspected tumors
- the appearance of purulent foci (abscesses, phlegmons),
- hematomas and soft tissue ruptures,
- preparation for operations,
- control over recovery after treatment.
Sonography can detect a tumor, but it cannot determine whether it is benign or malignant. To clarify the diagnosis, patients are additionally prescribed Doppler ultrasound or biopsy.
The only limitation for soft tissue ultrasound is the open wound in the area of interest. The procedure has no other contraindications.