In terms of frequency, various diseases of the genitourinary system have not yet “caught up” with neurological or cardiovascular diseases, but they are surely approaching them. A variety of infections, predominantly sexually transmitted, bacteria, the number, variety and danger of which are growing every day, all contribute to the manifestation of certain diseases. They can be identified by bladder cystography - a procedure that is equally successful in men and women and has a reputation for being a highly accurate examination.
What is cystography?
Cystography: what is it? This type of X-ray examination of the body has been used by medical specialists for quite a long time. Its essence lies in the introduction of a special substance - contrast - into the human bladder and subsequent X-ray imaging of the organ. Cystography is a method that has gained popularity due to its high information content, as well as affordability. Unlike magnetic resonance imaging (MRI), which requires the medical institution to have sophisticated equipment and the patient to have a sufficient amount of money, a cystographic examination does not require such costs.
How is cystography done in children?
For a newborn or older child, cystoscopic examination is prescribed in extreme cases. The volume of contrast agent for a child is 50-100 ml. Children over 13 years old are given 200 ml of contrast.
When the doctor takes pictures, parents or medical staff must fix the child in a stationary position (the image will be blurred when moving). After the bladder has emptied, final images are taken. In this case, the shoulders and legs must be raised at a right angle.
After the procedure is completed, the doctor analyzes the resulting images. If necessary, additional tests are prescribed, which together makes it possible to detect the presence of oxalates or other deposits in the urine. An X-ray image shows the contours and shape of the bladder, thickening of its walls, the presence of tumors, cysts and other structural changes in the organ.
Based on the information received, appropriate treatment is prescribed. This may be a course of drug therapy, dietary nutrition, hospital treatment or surgery (if ruptures or tumors are detected).
Types of cystography
There are several types of diagnostics; they can be carried out either individually or in combination. Sometimes the examination complements other x-ray studies, for example, urethrography. This is widely used by doctors who find it difficult to make a definitive diagnosis in the case of rare forms of a particular disease.
Ascending cystography
Ascending cystography is a method in which the bladder is filled with a contrast agent directly through the urethra. The procedure is extremely informative and helps to identify many diseases even at their initial stages. The only disadvantage of the diagnosis is the discomfort that the patient may experience during medical procedures.
Descending cystography
Descending cystography differs from the previous examination method in that the contrast is not injected into the bladder, but intravenously, after which it is excreted by the kidneys. This option is less reliable because it can give a false result, and therefore is often used in combination with other types of x-ray examinations. The method is also less popular due to its long duration: first, the diagnostician must wait for the contrast to reach the kidneys through the blood, and then until it reaches the bladder.
Vaccine cystography
Another method is voiding cystography of the bladder, it makes it possible to understand what is happening not only in the bladder, but also in the urethra: such an examination assumes that an x-ray will be taken at the time of urination.
How is cystography done in women and men?
Before the procedure begins, the patient lies with his back on the X-ray machine. After this, several photographs are taken to help assess the location and condition of the peritoneal organs. A contrast agent is then injected through the catheter. When the bladder is full, the catheter is clamped. It is this moment that becomes the most unpleasant and uncomfortable for the patient.
After filling the bladder, the doctor takes several pictures from different angles: on the sides, stomach, back. To get a clear image, the patient needs to raise his legs at a right angle. The bladder is then emptied and a final image is taken without staining agent.
For women, the procedure is much simpler and less painful than for men. This is due to the anatomical features of the female ureters - in women they are wider and shorter. In men, the urethra is much narrower and longer, so inserting a catheter is more problematic. In men, it is recommended that a descending radiocontrast study be performed using intravenous contrast. Thus, the diagnosis will not cause pain or discomfort.
Indications for use
Thanks to cystographic diagnostics, specialists have the opportunity to monitor a variety of diseases of the genitourinary system: from the least significant to serious ones that require prompt surgical intervention or intensive drug therapy.
If you suspect tuberculosis of the genitourinary system
A disease such as tuberculosis affects not only the respiratory but also the human genitourinary system, which not every patient knows about. In order to prevent the disease from affecting as many tissues as possible and then spreading to other organs, which will lead to death, cystography of the bladder should be performed when the first alarming symptoms are detected. These include: increased blood pressure, pain when urinating, blood in the urine (not always).
If you suspect stones or sand in the bladder

An X-ray of the bladder is also informative in case of urolithiasis. This is a common disease that affects middle-aged and elderly people. It is characterized by acute or dull pain, frequent urge to empty the bladder, and general malaise. Without timely medical care, it leads to the death of the kidney. Cystography of the bladder in women and men can also reveal sand in the bladder - a condition accompanied by pain, a feeling of incomplete emptying when urinating and other unpleasant symptoms.
Detection of congenital pathologies of the urinary system
Congenital pathologies today are diagnosed already in childhood, in the first days and weeks of life. They can either cause no discomfort or cause serious physical and even mental disorders. Most require surgical intervention.
If vesicoureteral reflux or serious bladder injury is suspected
Vesicoureteral reflux is a pathology characterized by the reverse movement of urine (from the bladder to the ureters), which leads to the development of inflammatory processes and infection. May be congenital or acquired as a result of injury. Adverse physical effects on the bladder can also cause problems in its functioning.
Possible consequences of cystography
Cystographic examination is a painful procedure that can provoke the development of a number of complications. Therefore, this procedure is prescribed in extreme cases. Side effects of cystography include:
- Allergic reaction to the administered substance. Signs of an allergy may include skin rashes such as hives or difficulty breathing. To normalize the condition, hormonal drugs are administered intravenously.
- Nephrotoxic syndrome, which occurs against the background of allergies. Its manifestations include dizziness, severe headaches, and the smell of acetone from the mouth. This situation requires serious medical intervention and detoxification treatment.
- Traumatic damage to the bladder during catheter insertion.
- Reflex spasm of the sphincter (urinary retention). Typically, this complication occurs in older men.
In children, after cystoscopy of the bladder, the following consequences may occur:
- Injury to the mucous membrane, which is accompanied by bleeding when urinating for several days after the procedure;
- Exacerbation of pyelonephritis. To prevent such a complication, the child is prescribed uroseptic medications before cystoscopy;
- Intolerance to the contrast agent used during the study. Allergies manifest themselves in the form of hives, difficulty breathing, swelling and shortness of breath. Before starting cystoscopy, the doctor must prepare special medications in case of an attack.
To avoid the development of these side effects, the patient should carefully follow the rules of preparation for the study and follow all the doctor’s instructions.
Attention!
This article is posted for informational purposes only and under no circumstances constitutes scientific material or medical advice and should not serve as a substitute for an in-person consultation with a professional physician.
For diagnostics, diagnosis and treatment, contact qualified doctors! Number of reads: 7001 Date of publication: 11/17/2017
Urologists - search service and appointment with urologists in Moscow
Preparation for the procedure
If you have an indication for cystography, then two days in advance you need to start preparing for the procedure for an x-ray of the bladder
. First of all, you need to exclude legumes, raw vegetables, brown bread, as well as fruit and vegetable juices from your diet. These products cause increased gas production, which may lead to false results. If you smoke, reduce the number of cigarettes you smoke during this time.
Immediately before visiting the diagnostic room, you must empty your bowels and do an enema.
Carrying out cystography
How is bladder cystography done? With the ascending method, the patient lies down on an X-ray machine and a catheter with contrast is inserted into his urethra. If necessary, local anesthesia is possible. The person is then asked to change their body position several times. For downward diagnosis, an intravenous injection of a contrast agent is performed. Vaccination cystography is also performed using a catheter, after which the patient is asked to empty the bladder.
Type of cystography
The cystographic examination procedure is performed using a catheter. With its help, the bladder is filled with 150-200 ml of a special solution, which consists of 10-30% of a radiopaque substance (urografin, iododamide, triomblast).
The drug is administered in two ways - ascending and descending. The ascending route involves the introduction of contrast through the urethra (urethra). Descending is carried out by injecting a contrast agent into a vein.
The listed types of examination are not always sufficiently informative, since they do not allow the detection of non-contrast stones and tumor growths. For a more detailed diagnosis, the doctor may recommend pneumocystography. It differs from cystography by using a gas (nitrous oxide, oxygen or carbon dioxide) instead of a contrast agent.
In some cases, a combination of two methods of filling the bladder is performed. First, 15-20 ml of contrast and 200-250 cm³ of gas are injected. This type of study is called lacunar cystography. Another type of X-ray contrast diagnostics is voiding cystography. Assessment of the functioning of the urinary tract in this case is carried out during the process of urination.
Contraindications
Not every patient is allowed to undergo a cystographic examination. First of all, the ban applies to allergy sufferers. In the cases below, other types of diagnostics are also chosen.
The presence of blood in the urine (the diagnostician may mistake clots for stones)
This symptom is characteristic of some infectious and inflammatory diseases, as well as increased blood clotting.
Education and inflammation in the genitourinary organs
If, during tests and other diagnostic methods, the doctor discovered a cyst, benign or malignant tumor, or identified an acute inflammatory process, then cystography will have to be abandoned.
| To main |
(Radiation diagnostic news 1998 3: 29-31)
Radionuclide diagnosis of vesicoureteral reflux.
Stolin A.R., Makarevich V.F., Ermolenko Yu.A.
Mogilev regional hospital.
Vesicoureteral reflux (VUR) is a very dangerous disease that can manifest itself in early childhood with uncharacteristic symptoms. Undoubtedly, a considerable proportion of cases of VUR tend to spontaneously heal, either without consequences or with a defect in the form of persistent dilatation of the ureter and pelvis. In another part of patients, however, undiagnosed and, therefore, untreated PMR leads, due to recurrent urinary tract infections, although sometimes without them (the so-called “sterile reflux”), to scarring of the renal parenchyma, the development of hydronephrosis with impaired renal function, and - in serious cases and to loss of organ function. A common complication of PMR is the development of renin-dependent arterial hypertension. Bilateral reflux can cause renal failure and uremic death.
X-ray voiding cystography is still considered the most popular method for diagnosing and monitoring VUR. The main advantages of this method are to obtain information about the details of the structure of the bladder and the anatomy of the urethra, as well as the ability to classify VUR in accordance with accepted criteria. However, a significant radiation exposure to a child, especially dangerous in girls due to the impossibility of shielding the gonad area, forces us to look for alternative approaches to diagnosing this common disease. In addition, being “discrete,” the X-ray method cannot guarantee that PMR, the manifestations of which in many cases are also very limited in time (seconds!), will certainly coincide with the moments when the images were taken.
When choosing treatment tactics, clinical data, the severity of VUR, the state of separate renal function, involvement of the ureteric orifices, and the presence of scars in the renal parenchyma are assessed. Many important questions that arise both during the initial diagnosis of PMR and during dynamic monitoring of the patient are answered by radionuclide tests - indirect and direct cystography. Both of these methods were mastered for the first time in the republic in the radionuclide diagnostics laboratory of the Mogilev Regional Hospital and, it seems to us, some of their aspects may be of interest to colleagues.
Indirect (intravenous) radionuclide cystography.
For the study, 99mTc-MAG 3 (mercaptoacetyltriglycine) or 99mTc-DTPA (diethylenetriamine pentaacetate) is used. We use DTPA drugs - Pentatech (Diamed, Russia) and Pentetate (Amersham, England). The procedure is carried out in accordance with a modified protocol proposed by A. Bockisch and R. Piepenburg [1].
First, dynamic nephroscintigraphy is performed according to the generally accepted method after intravenous administration of 1.5 MBq 99mTc-DTPA per 1 kg of the child’s body weight and previous hydration. Recorded serial twenty-second images are processed using standard computer programs, as a result of which information can be obtained on the morphology of the kidneys and urinary tract, as well as, by constructing activity-time curves from selected areas of interest, information on individual renal function.
Immediately before the study, it is very important to empty the bladder, since in a full bladder the concentration of the tracer released into it will be significantly lower, which will significantly reduce the sensitivity of the method in a subsequent attempt to detect PMR. After completion of dynamic nephroscintigraphy, which usually takes 20 minutes, the patient is instructed not to urinate for as long as possible. The patient is periodically tested using a gamma camera, waiting for the upper urinary tract to empty as completely as possible from the mark. After this, he is again seated with his back to the detector plane of the gamma camera, using a special chair with a reinforced urinal. Start recording two-second images of the urinary tract. On command, 30 seconds from the start of registration, the patient urinates; Meanwhile, image recording continues. It ends 4 minutes from the start. Thus, we receive 120 two-second images - before the start of the miction, during and after it. When computer processing the received information, we select areas of interest - from the kidneys, ureters and bladder - and construct activity-time curves. A pronounced rise in the curve above the kidney or ureter, synchronous with voiding, indicates the presence of VUR.
In small children who are not available for contact, miction on command can be replaced by pressure on the bladder area. Image registration in such patients is carried out in the supine position; in rare cases, they resort to sedation of children during the study.
The undoubted advantage of indirect radionuclide cystography is the ability to quantitatively assess the structure and separate function of the kidneys, the absence of the need for bladder catheterization, and the physiological nature of the test (the urethra is not irritated by the catheter, and the bladder is not irritated by the injected solution, which is the case with X-ray and direct radionuclide cystography). The radiation dose to the patient and, in particular, the gonadal dose is significantly less than during corresponding x-ray procedures.
The method, however, has a number of disadvantages. The main one is low sensitivity. Although, according to some estimates [2], there is a good correlation between indirect radionuclide cystography and X-ray voiding cystography, perceived as the “gold standard,” most researchers [3, 4] assess the sensitivity of the test as very low with a significant percentage of false negative results. In addition, although the radiation dose to the patient, as already mentioned, is low, it is still much higher than with direct radionuclide cystography, and in cases of impaired renal drainage (which is a common finding in PMR), the radiation dose to the kidney can be noticeable.
Finally, the results of the method depend on renal function, as well as on the possibility of cooperation with the patient during the study: sometimes children cannot urinate in an unusual environment, and delayed miction results in excessive radiation exposure to the bladder wall.
To summarize, we can recommend indirect (intravenous) radionuclide cystography for dynamic monitoring of already diagnosed VUR, but not for its primary diagnosis (the exception is patients with a single kidney, for whom endovesical manipulation is extremely undesirable). When assessing the test results, one can be guided by the rule: positive results are reliable, while negative results should be rechecked using direct cystography if there is serious suspicion of the presence of VUR.
In Fig. 1
The curves of patient Z., 8 years old, are presented. It is clearly visible how, simultaneously with the onset of miction (curve 1, recorded above the bladder), activity clearly increases over both ureters and both kidneys (the remaining curves) - a typical picture of bilateral VUR.
Direct (retrograde) radionuclide cystography.
When carrying it out, we are guided by the protocol proposed by M. Majd [4]. In general, it involves catheterizing the urethra, retrogradely filling the bladder with a saline solution of sodium chloride mixed with a tracer, and obtaining images of the urinary tract area using a gamma camera during bladder filling, at the time of urination, and after it.
The patient is placed on his back on the gamma chamber table, placing a plastic diaper under the pelvic end to avoid contamination of the table with 99m-technetium. The urethra is catheterized under aseptic conditions using a Foley catheter or plastic feeding tube for newborns. The bladder empties.
The catheter is connected to a bottle of saline sodium chloride solution warmed to body temperature using an intravenous infusion system. The bottle is placed at a height of 100 cm from the table surface. Once the fluid flow has stabilized, 37 MBq of 99mTc sodium pertechnetate is injected into the gum. The patient is positioned so that the bladder is projected at the lower edge of the persistentscope screen and computer monitor. At the moment of detection of reflux, it is noted at what volume of the bubble it appeared (this data will be very important during dynamic monitoring of the patient and repeated testing). If bilateral VUR is detected, fluid administration into the bladder is stopped immediately. If reflux is not detected, the bladder is filled to a volume, which in children is determined by the formula: bladder capacity = (age in years + 2) x 30 ml.
We must remember, of course, that there is a bladder with a very small capacity (10 - 20 ml!), as well as the fact that children prone to infrequent urination may have a bladder capacity exceeding 500 ml. In general, sufficient filling of the bubble is indicated by the cessation of fluid flow when the bottle with saline solution is lowered to a level of 30 cm above the bubble.
Once the bladder has filled, the catheter is removed and the patient is encouraged to urinate. Very young children urinate in their diapers while remaining on the table.
Older patients urinate while sitting with their back to the detector plane. In any case, it is important that the entire process of filling the bladder, miction and the state of the urinary tract after urination are continuously recorded by a gamma camera. A series of ten-second images is obtained, as well as one-minute images throughout the study.
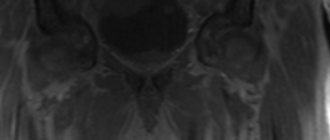
In Fig. 2
The processed image shows left-sided VUR during the filling phase of the bladder.
The described method has a number of important advantages. The main one is the extremely low radiation dose: less than 15 mrad on the bladder wall and less than 5 mrad on the ovaries. The testicular dose does not exceed 2 mrad. At the same time, the gonadal dose with standard x-ray voiding cystography ranges from 75 mrad to several rads (!), depending on the study conditions and the number of images. Further, even a very short PMR will not be missed when performing direct radionuclide cystography, unlike X-ray. Thirdly, with the radionuclide method, neither bone structures nor intestinal contents interfere with the detection of even small reflux, which often complicates the assessment of x-ray cystography.
The volume of the bladder at the time of the appearance of VUR, as already mentioned, has considerable prognostic significance in repeated studies. Finally, the method makes it possible to quantify the volume of both reflux and residual urine.
Disadvantages of the method are the inability to assess the anatomy of the male urethra (therefore, performing the test in boys is not recommended without first studying the characteristics of the urethra during urination as part of routine excretory urography), insufficient resolution, which sometimes makes it difficult to assess the degree of VUR, and the need for bladder catheterization.
The combination of the high sensitivity of the test and low radiation exposure allows us to recommend it as the method of choice: a) for dynamic monitoring of children with already diagnosed VUR or who have undergone antireflux surgery; b) as a screening study for detecting reflux in asymptomatic siblings of children diagnosed with VUR; c) in serial studies of children with a neurogenic bladder and a high risk of developing reflux; d) for primary screening of girls with urinary tract infection to detect possible reflux; e) for the same purpose in boys after a preliminary study of the anatomy of the urethra.
It seems to us that the described methods for diagnosing and monitoring PMR deserve to be widely used in specialized hospitals in the republic and should, at least in part, displace X-ray voiding cystography from pediatric practice.
Literature:
1. A.Bockisch, R.Piepenberg. Der Nuklearmediziner, 1994, 2, 155-163. 2. I.Gordon, AMPeters, S.Morony. Pediatr. Nephrol., 1990, 4, 604-606. 3. M. Majd, E. J. Kass, A. B. Belman. Ann. Radiol., 1985, 28, 322-328. 4. Diagnostic Nuclear Medicine, ed. by MPSandler et al., Williams & Wilkins, 1996, 3rd ed., vol. 2, pp.1369-1398.
| Rice. 2. Direct (retrograde) radionuclide cystography. Vesicoureteral reflux on the left. | |