Briefly about the diagnostic method
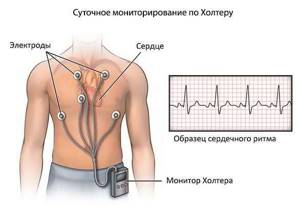
Holter monitoring is a long-term recording of an electrocardiogram, a method for diagnosing heart damage, proposed by the American biophysicist Norman Holter.
Long-term recording of an ECG allows one to evaluate the work of the heart during the patient’s normal life, under various loads and taking medications. Holter monitoring is a continuous recording of an electrocardiogram for 24 hours or more. The electrocardiogram is recorded using a special portable device (recorder), which the patient carries with him (on a belt over his shoulder or on his belt). Recording is carried out on several (up to 12 channels), but more often on 2 or 3 channels.
Types of Holter monitoring
There are two main types of this survey:
1. Fragmentary . It is carried out to record an ECG during arrhythmia and is prescribed on an outpatient basis for rare attacks. Basically, short-term recording is used when the patient, feeling worse, starts recording on the monitor and turns it off after the symptoms disappear.
2. Continuous. The most common type of diagnostics with the duration of signal recording from 1 to 3 days. During this time, about one hundred thousand cycles are recorded. Some devices can analyze the QRS complex and also send electrocardiogram data to a diagnostic center, where a specialist interprets them.
There are also devices implanted into the body (installed and removed surgically) that can record ECGs for a long time (up to 14 months).
Interesting! All ECG monitors use disposable adhesive electrodes. At the same time, such sensors are produced with different diameters for adults and children.
Preparing for diagnosis
The installation time of the recorder will take no more than 10 minutes: attaching electrodes to the treated (shaved for men and degreased for all) chest skin - 5-7 pieces + cuffs on the shoulder, if blood pressure monitoring is provided. After attaching the device, the patient receives a diary with instructions to write down everything that will happen to him during a 24-hour wearing of the halter (night rest, exercise, eating, walking, psycho-emotional stress, doing household chores, watching a TV series or a football match, work matters, taking medications). In addition, in the issued diary, the patient records all his sensations (pain, discomfort, palpitations) under certain circumstances (stress, lunch, sleep, etc.).
Stages of preparation for the examination and features of its implementation
In order for the technique to show reliable results, the patient should prepare for a procedure that will last for 24 hours or 3 or more days. Before the procedure, it is necessary to take a shower, because during the examination the patient must not remove the equipment or wet it with water. You should remove metal jewelry and accessories (watches, earrings, pendants), as metal negatively affects the accuracy of cardio readings. During the procedure, you need to wear comfortable clothes, preferably cotton.
For proper operation of the device, water should not be allowed to get on the equipment; contact of the equipment with other devices that create magnetic fields around them should be avoided. You must carry the recorder carefully so as not to damage its integrity: you must not drop or hit it.
The equipment consists of 2 parts - a stationary decoder and a recording device that takes readings. The electrodes are fixed to the skin.
A full-scale heart study is carried out while the patient leads his usual lifestyle, prepares food, runs, sleeps, eats, and rests. Everything that the patient does during the monitoring process is recorded in the diary. The time spent on a specific action is recorded. You can characterize your condition using three indicators: worsened, improved, or remained unchanged.
Rules and recommendations during a Holter ECG: first, you should not exhaust yourself with physical activity, because there is a risk that the electrodes will detach from the skin and the diagnostic results will be inaccurate: second, the patient should avoid stressful situations; third, it is undesirable to travel, fly on an airplane or go on attractions during the examination; fourth, the device should not be exposed to strong temperature changes; fifth, you should protect the recorder from moisture and water.
The patient should lie on his back so that the location of the electrodes is not disturbed. If your back hurts, you can turn over on your side, but at the same time monitor the operation of the device. This technique is considered safe; it does not cause complications or pathological changes. Cardiac registration should not be prescribed to people with high blood pressure, left ventricular diastolic dysfunction, organ dysfunction, acquired heart defects, asymptomatic myocardial ischemia, angina pectoris (chest discomfort).
Best materials of the month
- Coronaviruses: SARS-CoV-2 (COVID-19)
- Antibiotics for the prevention and treatment of COVID-19: how effective are they?
- The most common "office" diseases
- Does vodka kill coronavirus?
- How to stay alive on our roads?
How is the diagnosis carried out?
Modern devices for long-term ECG recording are electronic devices with a large memory capacity. The electrodes are fixed on the patient's body using a special adhesive patch. Wires from these electrodes lead to a monitoring device. During the registration of the electrocardiogram, the patient leads his usual lifestyle, noting in a special diary the time and circumstances of the occurrence of unpleasant heart symptoms, taking medications and changing types of physical activity. The doctor can give the patient tasks, for example, to climb a certain number of steps and mark the completion of the task by pressing a button on the monitor. In this way, the doctor will be able to analyze changes in heart function during physical activity.
What is Holter
During the examination, a special portable device is used - Holter. Its electrodes are attached to the patient’s chest; they record all changes in blood pressure and record an ECG throughout the day.
The diagnostic device is named after Norman Holter, a famous American biophysicist researcher. In 1961, he developed a monitoring technique and put it into practice for the first time. Thanks to the Holter method, today cardiologists can identify disturbances in the functioning of the heart and various hidden diseases that are not visible on a regular electrocardiogram.
After diagnosis
The analysis of the received recording is carried out on special decoder computers. When deciphering, information about the heart rhythm is indicated: its source and frequency; information about rhythm disturbances: supraventricular and ventricular extrasystoles, paroxysms of arrhythmias; information about rhythm pauses; information about changes in the PQ and QT intervals, if these changes occurred, information about changes in the morphology of the QRS complex caused by intraventricular conduction disorders; information about changes in the final part of the ventricular complex (ST segment) and the connection of these changes with the patient’s physical activity and his feelings according to the diary; information about the operation of the artificial pacemaker - if there is one. Identified features or pathology can be illustrated with ECG printouts for the corresponding monitoring period.
Memo for the subject
To achieve the most accurate result, you must follow the following rules:
- Use clothes made from natural fabrics. No metal elements or too loose clothing.
- Maintain the temperature of the device at average values
- Do not allow the device to come into contact with liquids
- Do not expose the device to vibrations
- Keep a distance from transformer boxes and similar structures
- Limited use of mobile phones and other similar devices.
- Do not subject the device to deformation
- Monitor the position of the electrodes on the body
- Determine the possibility of physical activity
Possible complications
In terms of diagnosing coronary heart disease, the results of Holter monitoring cannot reliably exclude pathology of the coronary arteries. If a certain suspected phenomenon is not detected during Holter monitoring, this does not prove the absence of this phenomenon in the patient. In general, Holter monitoring is an important auxiliary diagnostic method that allows you to confirm the cardiologist’s suspicions of cardiac arrhythmias and coronary circulation disorders.
Who should use monitoring?
Most often, the electrocardiography procedure is prescribed for the following problems:
- unpleasant chest pain
- cardiopalmus
- frequent dizziness
- breathing disorder
- fainting
If a routine ultrasound does not show any abnormalities for these concerns, then most likely the doctor will prescribe Holter monitoring.
If paroxysmal tachyarrhythmias are suspected, this method of diagnosing the disease is important, since the attacks are intermediate in nature.
This disease is accompanied by other ailments:
- angina pectoris
- microinfarctions
- Congenital heart defect
Daily monitoring does an excellent job of monitoring the effectiveness of treatment for a particular disease.
Contraindications Holter monitoring
This type of examination is absolutely painless and simple. Following the rules described above, monitoring will not bring much discomfort in everyday life.
This type of procedure can be performed during pregnancy, breastfeeding, as well as in childhood and old age.
Monitoring has no contraindications or side effects.
What information can be obtained using Holter?
Conventional electrocardiography is not always able to provide the necessary information about the functioning of the cardiovascular system, due to the fact that it is carried out over a certain period of time. At the same time, various attacks of arrhythmia can be observed only at specific moments, and during examination in the clinic they may not manifest themselves at all.
Therefore, 24-hour Holter monitoring is considered a very valuable diagnostic method. Using the device it is possible to obtain the following information:
- stability of the heart in conditions familiar to a person, which makes it possible to record reactions to physical activity, emotional stimuli, etc.;
- cardiac conductivity during the day;
- the presence of arrhythmia attacks and the degree of their danger;
- identification of episodic manifestations of myocardial ischemia.
Thus, the use of Holter in Voronezh allows specialists at the OKO clinic not only to make an accurate diagnosis, but also to evaluate the effectiveness of the current treatment method and the need for its adjustment.
Indications for the use of Holter monitoring
This diagnostic method is used for patients in the following cases:
- the need to assess the effectiveness of prescribed treatment measures;
- to establish the causes of arterial hypertension and prescribe quality treatment;
- some conditions that may be consequences of cardiac dysfunction (for example, rapid heartbeat, loss of consciousness);
- monitoring the patient’s condition after a heart attack;
- presence of suspicion of angina pectoris;
- serious disturbances in the functioning of the endocrine system.
In these and a number of other cases, the use of this diagnostic method will be appropriate. At the OKO clinic in Voronezh, Holter is used to diagnose the state of the cardiovascular system of patients, since problems with the visual organ can be a consequence of cardiac pathology.
What is strictly forbidden to do during the study
During Holter ECG monitoring, special small sensors are attached to the patient’s skin in the chest area that record the electrical activity of the heart, as well as a small device (the dimensions of modern Holter devices are small, they are comparable to the size of an MP3 music player). To prevent malfunction of the device, disconnection of sensors, and obtaining erroneous results, you should avoid taking a bath or shower, change clothes frequently, and wear clothes with buckles, clasps, and metal jewelry (earrings, piercings). The device should be protected from excessive vibration and shaking. It is advisable to sleep on your back or side during the examination to avoid disconnecting the sensors. For high-quality operation of the device, it should not be exposed to humidity, high or very low ambient temperatures. You should also try to avoid excessive physical activity, which can lead to a significant increase in the functional activity of the heart and obtain erroneous test results. Since Holter monitoring itself in most cases lasts no more than 1 day, compliance with these restrictive recommendations is simple and not burdensome for the patient. The obtained reliable research results allow the doctor to establish an accurate diagnosis. In particular, effective treatment of arrhythmia, paroxysmal tachycardia, and mild blockade of certain areas of the cardiac conduction system is impossible without Holter monitoring.
Today, daily ECG monitoring is the method of choice for diagnosing pathology, which manifests itself only by periodic changes in the functional activity of the heart.
Decrypted data
On the results sheet you will see the following indicators.
| Index | Norm |
| Average heart rate during the day | 60–100 beats per minute |
| Average heart rate at night and during daytime sleep | 41–81 beats/min |
| Daily graph of heart rate changes | Changes when changing activities |
| Number of supraventricular extrasystoles | Up to 960 supraventricular extrasystoles per day (up to 40 pcs. per hour) A slight excess of the norm (up to 1200 pcs. per day) does not pose a threat to life and health |
| Number of ventricular extrasystoles | The absolute norm is 0. The permissible quantity that does not threaten life and health is 200 pcs. per day |
| The duration of the QT and PQ intervals and the schedule of their changes. | Normal QT interval: 340–450 ms (0.34–0.45 s) for women and 340–430 ms for men PQ – 120–200 ms |
Note! The norms indicated in the table are averaged and do not take into account age and individual characteristics of the body. Ask your doctor about the norm for you personally.