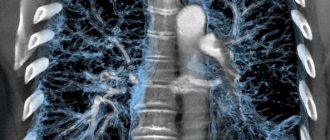
The pulmonary pattern is the network of vessels passing through the lung tissue. Normally, it is clearer at the roots of the lung and blurs as it moves away from them. This is due to a decrease in the diameter of the vascular lumen as they move away from the root of the lung. Normally, this pattern is more clearly visible in the lower lobes of the lungs, since the largest vessels are located there. X-rays do not show bronchi and lymphatic vessels.
What does it mean
The term “pulmonary pattern” refers to the display of the network of blood vessels that passes through the lung tissue. In a photograph of a healthy person, the vascular network at the roots is more clearly visible, since the largest vessels are located in this part. The closer to the border of the pulmonary fields, the paler the image - the vascular system of the lungs on the periphery is not clearly visible. An X-ray image may show deviations such as increased or deformed pulmonary patterns.
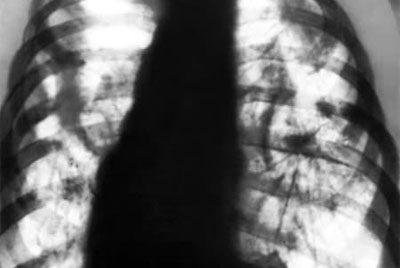
Normally, a fluorographic image looks like this:
- the clarity of the pattern of the left and right lungs should be the same;
- the branches of the vessels in the image should be straight;
- the general appearance of the image should resemble a butterfly in its outline, the branching of the vessels should be fan-shaped and even;
- the intensity of the display of vessels decreases from the roots of the lungs to the periphery and the shadows end approximately at a distance of 1/3 from the external borders of the chest;
- the thickness of the vessels in the fluorographic image should decrease evenly from the roots of the pulmonary system to the periphery;
- the vascular network should not be visible better than the shadows of the ribs.
The pulmonary pattern is formed by the arterial network, which emerges from the root of the lung. A healthy bronchopulmonary system is a network of vessels that evenly narrow from the hilar zone to the outer contours of the lung.
Reasons for increased pulmonary pattern on the right, left and lower sections
Before a conclusion is made about the reasons for the strengthening of the pattern, the patient’s age, his lifestyle and concomitant diseases are always taken into account.

Strengthening the pulmonary pattern in the lower sections is characteristic of segmental and lower lobe pneumonia.
Local changes are monitored at the initial stage of pneumonia, when vessels grow around the infiltrative focus. A similar picture is observed along the edge of the tuberculous conglomerate. Insufficiency of the lower section with endobronchial formation has similar symptoms, but the image must be analyzed carefully, since a mesh damage is formed.
An increase in the pulmonary pattern due to the interstitial (infiltrative) component may be the norm for a particular patient, and there is no point in worrying. This can be a sign of complications during the treatment of pneumonia. If a patient smokes for a long time, he develops chronic obstructive pulmonary disease. In half of former smokers, bronchial function is restored and the disease goes away. It is recommended to do spirography and make an appointment with a pulmonologist.
When the pulmonary pattern is enhanced due to the vascular component, this also indicates the individual characteristics of human physiology. Enlarged lymph nodes are possible, but this may be a symptom of other diseases.
In the case where the mixed type of shadow image is enhanced due to acute inflammation during bronchitis, pneumonia, cancer, and there are no characteristic signs, it is necessary to take a repeat image after two weeks and exclude oncology of the respiratory tract.
The structure of the lung tissue can be expressed due to the bronchial component during inflammation of the outer lining of the bronchi and occurs against the background of chronic bronchitis.

What does the term mean?
The principle of x-ray examination is based on the passage of ionizing radiation through human tissue, forming shadows and clearings. Shadows are formed as a result of ray retention in dense tissues such as bones, cartilage, and blood vessels. The lung tissue is airy; in the image, the fields look like areas of clearing with a mesh.
The pulmonary pattern is formed by vessels (arteries, veins) and main bronchi (main and 1-2 orders, which are formed by cartilage tissue), in appearance it resembles the branches of a tree crown, which disappear at a distance of 1-2 cm from the pleura.
Normally, these branches are thin and barely noticeable. In the presence of pathological processes in the lung tissues, in conclusion they write about an increase in the pulmonary pattern.

The symptom is subjective and can be interpreted differently by radiologists. The degree of enhancement largely depends on the radiation dose, the contrast of the image and the qualifications of the diagnostician.
A radiological symptom is considered to be a pathology in combination with clinical signs and in the presence of other radiological phenomena.
When is an increase in pulmonary pattern observed?
Local enhancement, accompanied by deformation, is easily diagnosed - just compare the drawings of the opposite lungs. Such changes often indicate inflammatory diseases. Often this indicates the initial stage or, conversely, prolonged pneumonia, pneumosclerosis caused by limited suppuration in the lungs, tuberculosis.
It is important that the clinical picture is not always clearly expressed - intoxication is often mild, and there is a cough with mucous or purulent sputum.
Despite the fact that the bronchi are deformed and brought closer together on radiography, they remain passable, and bronchiectasis is often detected on bronchography. An increase in the pattern has been observed for a long time as a manifestation of residual effects after acute pneumonia - it persists for up to six months.
Strengthening the pulmonary pattern in children
When analyzing children's X-rays, there are some things to consider. Since the pulmonary fields are smaller than in adults, the disappearance of the vascular network is observed not 1-2 cm from the edge of the lung fields, but at 0.5-0.7 cm.
Isolated basal strengthening is the norm in childhood, since the intensive growth of a child requires increased metabolism, therefore, respiratory movements in babies are more frequent: up to a year - up to 25-35 times per minute, while in an adult - up to 20. This requires increased tissue trophism lungs, improved blood circulation.
Deformation of the pulmonary pattern
Increased display of the vessels of the pulmonary field does not always indicate the presence of some dangerous disease, just like deformation of the pulmonary pattern on fluorography. What are the differences between these two x-ray abnormalities?
- With an enhanced image, there is only an increase in the clarity of the display of the vascular network at the periphery and in the hilar zone of the lungs, but the branches of the vessels are straight and regular.
- When the pulmonary pattern is deformed, changes in the natural arrangement of its elements and their outlines are visible.
In an image with a deformed pattern, uneven shadows and boundaries of blood vessels are observed; in different zones, their outlines can change and expand from the roots to the periphery.

As in the case of enhancement, deformation can be determined in individual zones, or can spread over the entire surface of the pulmonary fields:
- local changes in the outlines and dilation of blood vessels most often indicate a recent inflammatory process;
- uneven contours of vascular branches over a long distance are observed in diffuse (extensive) pathological processes.
Strengthening or deformation of the vascular pattern on fluorography after bronchitis, pneumonia or ARVI is not constantly observed. This phenomenon usually disappears within a few weeks after complete recovery.
What does the strengthening of the pattern in a fluorographic image indicate?
Strengthening the pulmonary pattern is a clear image of the vessels along the entire surface of the lungs and their roots. The image clearly shows the pattern of the upper and lower lobes of the lung. This may indicate the course of such pathological processes:
- tuberculosis;
- oncological neoplasms;
- pneumonia;
- heart defect (congenital or acquired);
- acute, obstructive and chronic bronchitis;
- pulmonary edema;
- some occupational diseases – silicosis, pneumoconiosis.
Depending on the type and extent of the pathological process, the enhancement can be local or diffuse. Ailments such as focal pneumonia and malignant neoplasms are displayed on the image as one or several foci of inflammation. With such processes, the pattern is enhanced precisely in those areas where pathology develops. This is called local enhancement of the pulmonary pattern.
If an extensive pathological process occurs in the lungs, then the pattern is intensified over the entire surface of the bronchopulmonary tree, from the roots to the outer borders and on the periphery . Diffuse enhancement of the pulmonary pattern in the image may indicate the presence of diseases such as miliary tuberculosis, lobar pneumonia, chronic and obstructive bronchitis.
In what cases should you sound the alarm?
When a radiologist makes a conclusion “strengthening of the pulmonary contours,” there is no need to despair. Fluorography is considered a biased way to diagnose lung diseases, where everything depends on the qualifications and experience of the specialist. Therefore, mistakes are common. But if a specific disease is indicated, for example, pneumonia, tuberculosis, you should not delay treatment.
When the image shows an increase in the pattern of the hilar region of the lungs, this indicates an inflammatory process in the bronchi during colds and acute viral diseases. With diffuse amplification, the roots are compacted and in some places stringy.
Fluorography helps prevent the development of serious pulmonary diseases when symptoms are detected in the early stages. If the doctor has sent you for additional examination, you must not refuse or neglect treatment - this is fraught with complications. The norm for an adult is considered to be a condition when the pattern of the lungs is visible in all lobes, the vessels are not dilated, and there are no local darkenings.

Is X-ray diagnostics safe?
Despite the fact that the patient receives a certain dose of radiation, X-ray diagnostics remain completely safe. The fact that it is also inexpensive makes this imaging method optimal for most patients.
The availability of such a method does not mean the possibility of its uncontrolled use, and even the need for a repeat image does not always become an absolute indication for repetition.
In some cases, the doctor will prefer a different research method. All received radiation is necessarily taken into account and summed up - thus eliminating the possibility of “overdose” and causing harm to a person. However, each person must take care of himself independently - if he undergoes such examinations on his own initiative, it is mandatory to report them to the attending physician.
Associated symptoms and additional examination
With diffuse lung damage, which is observed on a fluorographic image, there are usually concomitant signs of the disease in the form of any of these symptoms:
- temperature increased to subfebrile levels;
- discharge of purulent or bloody sputum;
- severe shortness of breath;
- attacks of suffocation;
- pain in the heart area;
- high blood pressure;
- infrequent or worsening cough.
If fluorography shows an intensification of the pattern over large areas of the vascular network, the patient is sent for examination. Usually he is prescribed sputum, blood and urine tests, an ECG and a repeat X-ray examination.
When no other complaints and symptoms, except for increased vascular network in the image, are observed, the doctor evaluates the advisability of further examination. For small local deviations in the form of dilation of blood vessels in the root zone or deformations of the contours of the vascular network in smokers, the pulmonologist may prescribe a repeat X-ray examination or consider this to be normal temporary or age-related changes in the structure of the lungs.

An increased pulmonary pattern on a fluorographic image does not always indicate the presence of any health problem. Sometimes the vessels are dilated due to an inflammatory process. If extensive deformations are observed in the image, the patient is sent for additional examination to determine the cause of this deviation.
Reasons for increased pattern during examination of a healthy person

The pulmonary pattern can be enhanced even outside of the disease. It happens that deviations are visible only on a fluorographic image, but the person does not feel any accompanying symptoms. In this case, increased display of blood vessels in the root zones is not considered a sign of any disease. The clarity of the vascular network can be increased for the following reasons:
- natural age-related changes in the human body. The reason for the strengthening of the pattern may be increased blood pressure, taking vasodilators, etc.;
- recently suffered bronchopulmonary disease. Vessels in the hilar zones of the lungs can be clearly displayed in the image if a person has recently suffered from bronchitis, pleurisy, or even a common ARVI;
- individual structural features of the vascular network of the bronchopulmonary tree.
When a person has recently had a cold, a residual cough can provoke a slight inflammation of the bronchial tubes. Sometimes this is displayed on a fluorographic image as an intensification of the hilar pulmonary pattern. This does not indicate any serious illness and does not require careful diagnosis. It is enough to visit a doctor so that he can carefully listen to the lungs and rule out wheezing, and then treat the disease with prescribed medications.
How the pulmonary pattern changes during diseases
Since vessels and bronchi with the surrounding connective tissue participate in the formation of shadows, changes in the contour are almost always associated with pathologies of the respiratory and cardiovascular systems.
These include the following ailments:
- chronic bronchitis - the pulmonary contours in the fluorography image are enhanced in all fields, sometimes heavy, in advanced cases - deformed;
- pneumonia - in the initial stage and the first time after recovery, the pulmonary image is locally enhanced;
- respiratory disease with damage to the bronchi and acute bronchitis - an enhanced shadow image is determined, especially in the root zone;
- heart diseases causing stagnation of blood in the pulmonary circulation, heart failure - strengthening and enrichment of the pulmonary pattern is formed due to the plethora of blood vessels in the lower sections;
- bronchial asthma. Diffuse enhancement and heaviness of the pulmonary pattern are also determined. If pulmonary emphysema develops, the pattern becomes poorer. This is due to overextension of the lungs and increased airiness of the lungs, the roots are compacted.
For sarcoidosis
X-ray changes in pulmonary sarcoidosis appear in 90% of cases.
Sarcaidosis is divided into five stages:
- 0 – no symptoms;
- 1st – thoracic lymphadenopathy, the lung parenchyma is not changed;
- 2nd – lymphadenopathy of the roots of the lungs and mediastinum in combination with changes in the lung parenchyma;
- 3rd – the pulmonary parenchyma is changed, lymphadenopathy of the roots of the lungs and mediastinum is absent;
- 4th – irreversible pulmonary fibrosis.
In addition to the typical symptoms of sarcoidosis, there are also destructive forms of the disease, bullous changes in the lungs, and sudden pneumothorax.
For emphysema
Characteristic changes on a radiograph with emphysema in the form of increased airiness of lung tissue occur due to prolonged smoking, the consequences of bronchial asthma or working in harmful conditions (inhalation of dust).

The diaphragm descends, its right dome is at the level of the neck of the 10th...11th rib. There is expansion of the interribs or protrusion of the sternum.
In the case of severe emphysema, the diaphragm resembles a tent in shape; steps grow due to fusion and exposure at the site of attachment of the diaphragm to the ribs when it is flattened.
For tuberculosis
With tuberculosis, an X-ray shows an increased clot in the affected area, and the contours of the lung change locally. Often tuberculosis is combined with chronic and obstructive bronchitis, so local changes appear along with diffuse enhancement.
The focal type of tuberculosis is characterized by limited spread in the lung, lack of complications and mild symptoms, while infiltrative tuberculosis is not limited to a certain area of the lung tissue. These can be small or large infiltrates of an entire lobe, one or two lungs. The infiltrate is the focus of inflammation, around which lymphocytes and leukocytes actively gather.
SOURCES: https://diagnostinfo.ru/rentgenografiya/vnutrennie-organy/usilenie-legochnogo-risunka-na-rentgene.html https://idiagnost.ru/issledovaniya/rentgen/chto-znachit-na-rentgenogramme-legochnyj-risunok -usilen https://pulmono.ru/diagnostika/rentgen/usilenie-sosudistogo-risunka-na-flyuorograficheskom-snimke
What happens to frosted glass in the lungs after Covid?
Inflammatory lesions in the lungs tend to resolve on their own within 7-14 days after the pneumonia has stabilized. However, the coronavirus does not go away without leaving a trace. Lung damage leads to a decrease in pulmonary function - on average by 20-30%, but in severe forms of the disease the percentage may be higher. A serious consequence of COVID-19 is the formation of hard fibrous tissue - this pathology is called pneumofibrosis or pneumosclerosis.
The development of fibrosis contributes to the occurrence of shortness of breath. It can be observed both during physical activity and at rest. Also, the consequences of a severe form of coronavirus will be chest pain, attacks of dry cough, and dizziness.
If pneumosclerosis of the lungs is detected due to coronavirus, doctors insist on regular examinations by a pulmonologist. He may order a CT scan to monitor lung recovery. Rehabilitation is also an essential part of recovery from illness.